All eyes on Napier
The gorgeous city of Napier, which proudly showcases it’s rise from the devastation of the 1931 earthquake to become the Art Deco capital of New Zealand, turned on a splendid weekend for the 89th New Zealand Association of Optometrists conference.
Over 100 delegates were treated to a varied programme of education in a congenial, relaxed environment. Sadly, the absence of members employed by multinational companies who do not support such meetings means these professionals, many of whom are young and newly graduated, remain disconnected from the profession they have chosen. These optometrists are missing the opportunity to interact with their peers and contribute to their professional future.
NZAO President Rochelle van Eysden opened the conference with a quote from philosopher George Santayana:
“We must welcome the future, remembering that soon it will be the past; and we must respect the past, remembering that it was once all that was humanly possible.”
This became the theme for many of the lectures, wherein advanced technology was celebrated alongside cautionary notes on limitations and with emphasis on interpretation of multimodal presentations.
Keynote speaker Professor Allison McKendrick, Head of Optometry and Vision Science at Melbourne University, opened by applauding the increasing use of OCT in optometry, noting that over 75% of the optometrists in the room had access to OCT. She, however, sounded a cautionary note that this can lead to over-referral, particularly for glaucoma, since most potential glaucoma cases are stable and progress slowly. Overwhelming, public ophthalmology services can lead to those people who do have rapidly progressing glaucoma not being seen in a timely manner, which leads to poorer outcomes later, she said. Adding that those who are treated aggressively for glaucoma that was never likely to progress, must suffer the consequential side-effects of treatment.
Prof McKendrick illustrated her point by showing that some completely normal eyes can show abnormal RNFL on the OCT due to, for example, the optic nerve variation in position above or below the foveal fixation point. As the OCT references the blind spot, about 30% of scans fall outside the reference database. Prof McKendrick cautioned the need to use clinical judgement and not rely solely on the OCT. Other acquisition issues include poor image quality (for example, from dry eyes), poor image centration, significant head tilt, segmentation faults, or unusual anatomical features such as tilted discs. Prof McKendrick emphasised the importance of excellent training for the person taking the images to be able to defray these issues, particularly when comparing previous images.
In the future, we will see a return to more personalised medicine and structure-function mapping, she said. In the meantime, we must rely on previous experience and skill to interpret correctly.
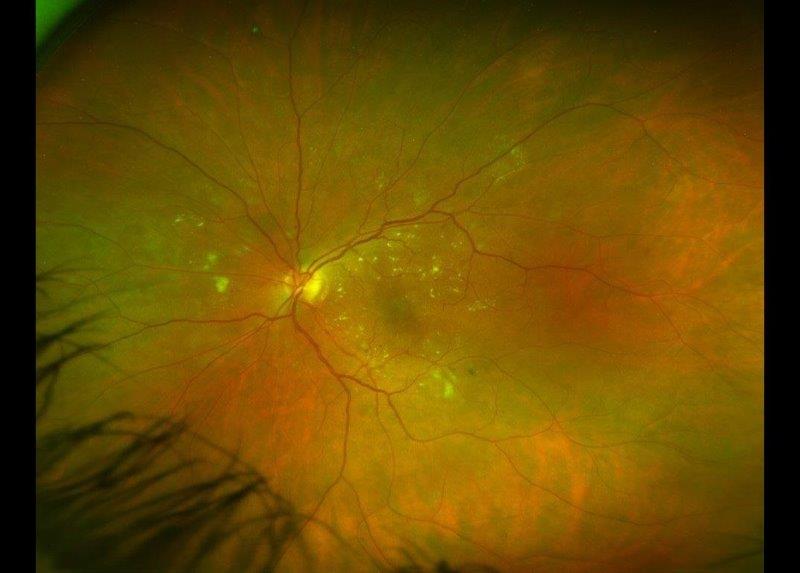
Dr Anjelica Ly continued a similar theme in her discussion of the role of imaging in monitoring AMD and predicting future progression. She asked the rhetorical question, “What tools do I have in my exam room to make my life easier?” I would prefer to rephrase that as “to make my patient’s life easier”, however, the answer lies in prognostic biomarkers. The word of the moment is prognostication, or determining who will lose vision and who won’t, based on four risk factors of drusen appearance and pigment. Again, the take home message was to use as many tools as you have at your disposal to identify progression. Applying evidence-based comparisons to catch late AMD early and imaging can be helpful in tying it all together.
Dr Jack Phu moved the discussion towards comparing visual field measurements. He showed that results between screening devices and different modes are not interchangeable, and that even repeated measurements on the same instrument can give spurious results. It can take many years to collect meaningful results to detect change, he stressed. Static automated perimetry does not give information on functional visual fields, which is what is of interest to patients in their daily lives, particularly among low vision patients. Peripheral and central visual fields need to be assessed separately particularly to predict function.
Joe Wang put our desire for the latest toys into perspective by showing us the trials and tribulations of bringing 21st Century eyecare to remote villages in the Himalayas. Technology for remote eyecare, otherwise known as ‘eyecare by smartphone’, opens up exciting avenues for providing services. There is an app for this, which is useful if you can keep the phone charged, find a way to manage a database where every surname is Sherpa and every first name is bestowed according to the day of the week you were born.
“Diversity asks, ‘who is in the room?’ Equity responds, ‘who is trying to get into the room and be heard?’”
Kiri Rikihana is a very interesting lady. A lawyer by training, she has a background in health law, governance and policy. She was previously a member of the ODOB and has recently become General Manager for the Australia and New Zealand College of Anaesthetists. With all her professional experience, it was her experience as a mother advocating for her child that she used to illustrate systemic inequality. She said, “Cultural safety is a mindset, not a tick box, but a way of thinking about personal power, privilege, education and how these effect how you got to where you are and how you interact with others. There is a changing landscape in NZ society which continues to evolve and emerge. Our health community is no longer willing to accept inequality of access, inequality in quality of delivery and unbalanced improvement for Māori.”
According to Kiri, equity relies on resources and we need to tailor resources in healthcare to match need. This requires thinking and doing things differently. Her final message to us was to call out racism and implicit bias in our society in general and in our organisations.
At this point one delegate was overheard to say to another “that was the best presentation on cultural competence and safety I have ever heard.”
Dr Graham Wilson, Gisborne ophthalmologist enthralled us with an update on the Dunedin Multidisciplinary Health and Development study, the world’s richest archive of human health and development. The eye and vision related part of the study is now starting to produce some fascinating longitudinal data.
Practical practice management tools were served up with breakfast by Eddie Quinones of MyHealth1st, a company that specializes in connecting independent optometrists with their patients. The Australian data shows that 70% of appointments are booked after hours. In NZ 35% of the on-line bookings are new to the practices using this technology.
Survivor Napier – a quizzical time
The first day ended with a fun session that involved everyone including exhibitors and families. Rochelle van Eysden hosted a pub quiz-style event and is to be commended for the effort she and her family put into this session, which segwayed smoothly into the drinks session, amid conversations and laughter.
Overall, this veteran of many NZAO conferences felt a sense of renewed energy and positivity with new blood in both the council and administration. Communication will be further improved by the suggestion of members having access to council via direct email, however if the strategic goal of reaching out to younger members is to be achieved, more attention may need to be given to social media and other relevant platforms.
So it’s goodbye from Napier and roll on Christchurch 2020!
Naomi Meltzer has worked in optometry for over 30 years and runs an independent, low vision consultancy service in Auckland. She is a MDNZ founding trustee.