Opinion: When steroids are not the answer
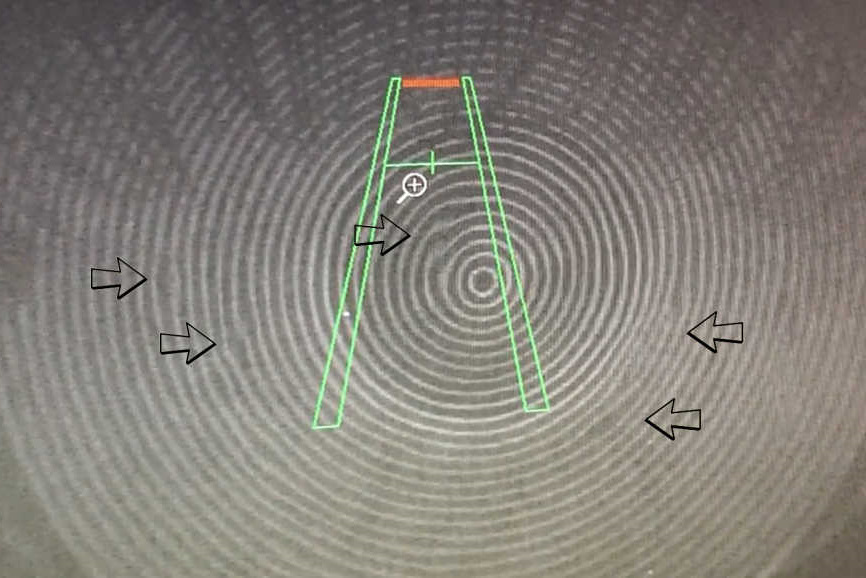
Here’s the thing many people don’t realise - dry eye is almost universally evaporative regardless of its cause. Even the rare aqueous deficient dry eye (eg. Sjögren's syndrome) has an evaporative component as well - unless patients have their eyes closed! Most often this hyper-evaporative component arises from co-existing meibomian gland dysfunction (MGD)1. With a functional lacrimal gland, most people with dry eye will thus have reactive epiphora from time to time and so the term, ‘tear film instability’, can often be intuitively better tolerated and understood by patients complaining of occasional watering.
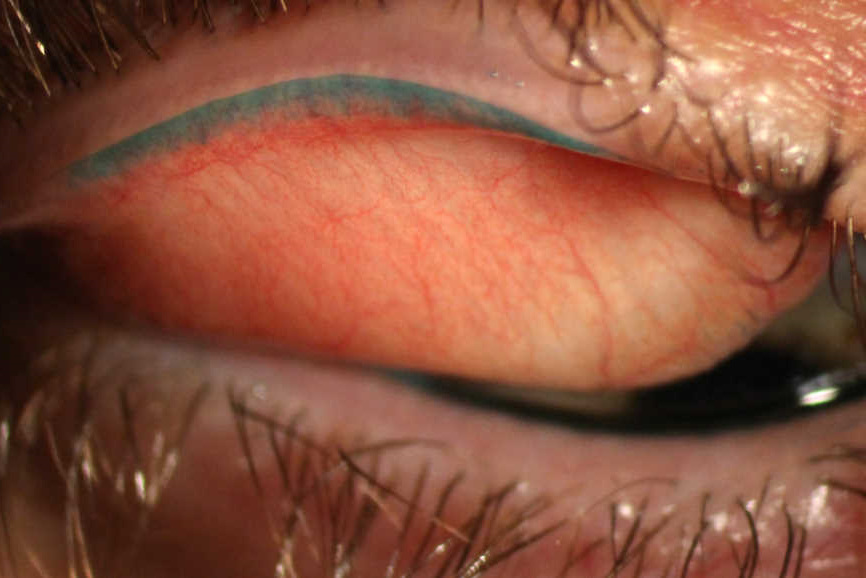
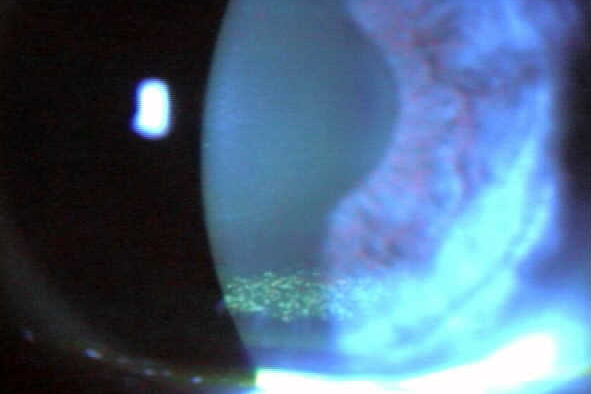
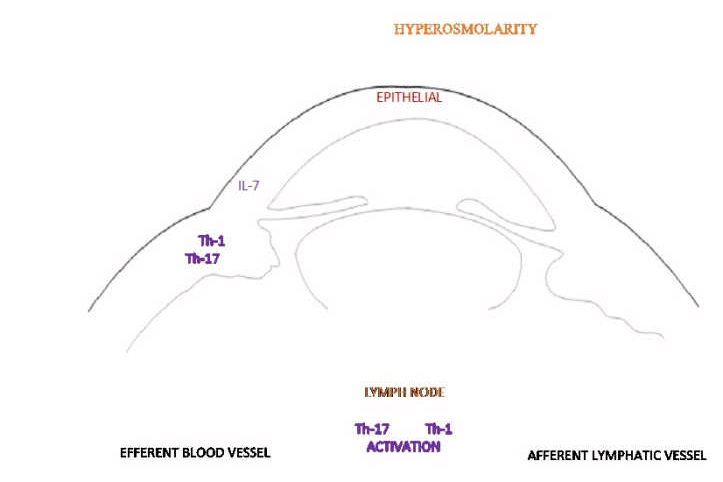
Due to a multitude of factors, including shearing forces, friction, underlying rosacea, rubbing, osmotic stress, iatrogenic stress from drops and preservative, there will usually be some level of inflammation present. While reducing the inflammation may be useful to improve comfort in the short term, it has to be remembered that inflammation is rarely the cause of the tear film instability. Making inflammation the therapeutic target is therefore not treating the dry eye.
We are yet to see drops that can stabilise the tear film with the longevity sought by patients. Lubricants have a largely palliative role, often simply replacing the aqueous layer of the tear film (and sometimes even flushing the lipid layer away). Treatment is therefore better targeted at improving tear film instability by promoting better lipid layer quantity and quality, with therapies such as hot compresses (42°C for 10 min daily is the current recommendation), intense pulsed light treatment, thermal pulsation (LipiFlow) or other methods that help promote an optimal tear film lipid layer.
About steroids
Inflammation reflects the body’s non-specific response to a whole host of insults - the final common pathway if you like. It is the healing response to damage or trauma. It is the defense to microbial assault or infection. In these settings, suppressing inflammation is not always beneficial and might even be downright counterproductive!
Even when warranted in cases of excessive inflammation, such as autoimmune disease, rosacea or allergy, steroids only temporarily suppress inflammation while they are being used. Steroids, by definition, are not targeted and have many effects including suppression of the immune system, altered metabolism, increased cataract risk, raised intraocular pressure, delayed healing etc.2, so they should only be considered when the benefits outweigh the risks and the side effects.
Steroids and dry eye?
Patients have an expectation they’ll be given drops for dry eye, but these typically provide symptomatic relief for only a few minutes. Artificial tear supplements and punctal plugs remain appropriate treatments for aqueous deficient dry eye which, as outlined above, is relatively rare; they don’t restore homeostasis of the tear film which is key to tackling dry eye.
If a patient is given drops and advised to perform hot lid massage daily for at least six weeks – the time it normally takes before any lasting effect is noticed – then there’s a risk the patient simply relies on their drops for short-term symptomatic relief and neglects the effective treatment, often resulting in them becoming frustrated both with their drops and they eye care professional!
Steroids are similar. Using steroids can result in symptomatic relief quickly, but this comes at the expense of identifying and treating the source of the inflammation. Thus, if a clinician instigates a short-term steroid regime for a chronic condition, such as dry eye, there needs to be a very clear understanding on the patient’s part that this is a short-term measure (one week) only. A solid plan of managing the underlying problem needs to be implemented while the steroids provide temporary relief. The risk of creating a steroid-dependent patient is quite high. So, in many cases, it is advisable to avoid prescribing steroids at the first consultation to allow patients to concentrate on treating their tear film instability before embarking on potentially, psychologically counterproductive symptomatic reliefs measures with risky steroid use. Chronic steroid use is not an option – the rule is, ‘only start them if you are brave enough to stop them!’
Alternatives to steroids
There are other options. Voltaren and Acular are relatively safe anti-inflammatory options if the patient has an intact corneal epithelium, and it may be that the small sting with NSAID drops even helps some patients judge and modify their own pain thresholds.
For Sjogren’s Syndrome or severe rosacea, where immune modulation is appropriate, cyclosporin or tacrolimus demonstrate superior safety profiles to steroids.
I firmly believe in targeted treatment. Steroids, to me, are the opposite of targeted treatment. So, before using any drop for dry eye, challenge yourself – ‘is this drop aiming to treat the condition or simply to provide symptomatic relief?’ If there is inflammation present – ‘what is causing the inflammation?’ If the benefit you achieve is purely symptomatic, does the patient fully understand this, because you need to think and discuss openly how you’re going to manage their chronic discomfort next year, and the year after that…
So, where do steroids fit in the treatment of dry eye? I would suggest they don’t. Emerging targeted treatments are rendering them almost obsolete.
References
- Sullivan DA, Dana R, Sullivan RM, Krenzer KL, Sahin A, Arica B, Liu Y, Kam WR, Papas AS, Cermak JM. Meibomian Gland Dysfunction in Primary and Secondary Sjögren Syndrome. Ophthalmic Res. 2018;59(4):193-205.
- McGhee, CNJ, Dean, S & Danesh-Meyer, H. Locally Administered Corticosteriods Benefits and Risks. Drug-Safety (2002) 25: 33
Dr Simon Dean is a consultant ophthalmologist with Counties Manukau District Health Board and the Eye Institute in Auckland, with specialist training in functional and cosmetic eyelid surgery and refractive surgery.