APSPOS 2025 inspiring collaboration
The third congress of the Asia-Pacific Strabismus and Paediatric Ophthalmology Society (APSPOS) was held in Brisbane from 29 June to 1 July. The theme, ‘Inspiring collaboration’, was clear from the start as it was held in conjunction with annual meetings of the Australian and New Zealand Strabismus Society (ANZSS) and the Australian and New Zealand Paediatric Ophthalmology Society (ANZPOS).
As I walked into the beautiful Brisbane Convention & Exhibition Centre, accents from around the world could be heard greeting old friends and making new connections. Orthoptists, optometrists, ophthalmologists and researchers from across the Asia-Pacific region and around the world gathered with the goal of improving paediatric eyecare globally.
With up to four sessions running at any given time, the biggest challenge was deciding which to attend. Each was packed with interesting topics and all beat a drum for collaboration.
Collaboration of skills
A New Zealand team of optometrists was asked to pair up with some Aussie orthoptists to run a practical workshop on paediatric glasses dispensing and Fresnel prism fitting… at an ophthalmology conference! This 90-minute session was well attended by a range of conference delegates and focused on the importance of getting the basics correct. Successful treatment of children who need glasses is reliant on every step in the chain working, which includes ophthalmology diagnosis, optometrist refraction, orthoptic work-up and appropriate dispensing. A range of frames and lenses was displayed with a detailed focus on frame requirements for paediatric suitability as well as how to get the best out of lenses.
The review of Fresnel prisms reminded me of how easy the options are to use and trial for patients, whether that is prior to surgery or specially made glasses, and encouraged me to use them more.

Just some of the Kiwi delegates: (back row) Dr Mary Jane Sime, Liz Gately, Drs Cam Loveridge-Easther, Stuart Carroll, Elizabeth Conner and Derek Sherwood and Noirin Kelly, Miriam Langeslag-Smith and Natalie Anton; (middle row) Sally-Anne Herring, Drs Julia Escardo-Paton and Justin Mora, (Skippy the Kangaroo), Tammy Miller, Mij McPhee, Drs Jay South and Rebecca Findlay, Lora Parson, Drs Rasha Altaie and Reid Ferguson; and (front row) Dr John Dickson, Federica Ferruzzi, Dr Samantha Simkin, Hamza Ali, Dr Cheefoong Chong and Nia Stonex
Another great example of skill collaboration was the work on congenital cataract management. Presentations discussed the group effort tackling screening programmes, surgical timings and techniques, plus amblyopia management with refractive correction and patching. Two stand-out presentations on this topic came courtesy of ophthalmology registrar Dr Leanie Leeson, who shared the management protocol and outcome differences for monocular and binocular cataracts at Queensland Children's Hospital, and optometrist Elspeth Wrigley, one of Queensland’s key rigid gas-permeable-lens fitters for infants and children. She explained the excellent oxygen permeability, low incidence of microbial infections and ease of access for patients. Screening, surgery or refractive correction alone do not improve visual outcomes for congenital cataracts – a team approach is necessary to maximise vision, Dr Leeson said.
Collaboration of countries
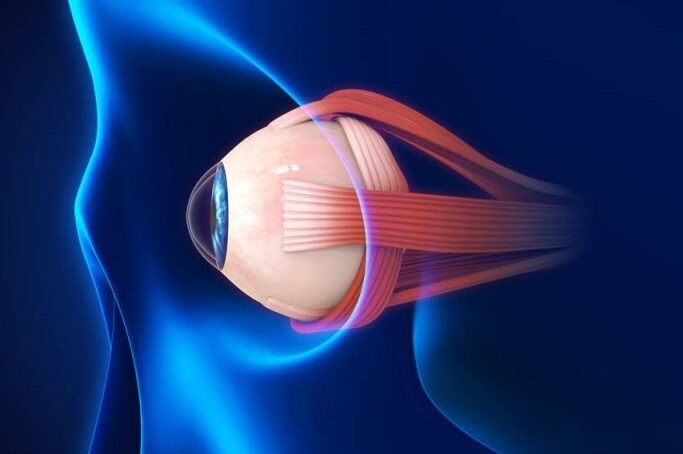
A session on ocular disease in systemic illnesses, hosted by the World Society of Paediatric Ophthalmology and Strabismus (WSPOS), was one of my favourites. The chairs, Dr Ken Nischal from Pittsburgh, Pennsylvania, and our very own Dr Elizabeth Conner, from Christchurch, highlighted the key role of the eye in determining diagnoses for children.
My takeaways were the importance of reviewing the whole child and referring for support in cases where this is not possible. Unique cataract presentations, abnormal optic nerves, keratoconus and corneal deposits can all be signs of syndromes or systemic diseases that need further assessment and scanning. Collaboration between eyecare practitioners, paediatricians and other health professionals, with clear communications of findings, can make the difference in reaching a diagnosis and, in some of the extreme presentations given, save a life. This encouraged me to strengthen my inter-professional relationships so that, when needed, help to a patient can be seamless and timely.
Collaboration on cases
Another highlight was the Tuesday morning live patient session. The local Queensland team had organised a group of patients living with challenging and unique cases of strabismus, many of whom had a history of multiple surgeries, ongoing double vision or simply did not know what to do next.
The expert panel of strabismologists included Professors Jonathan Holmes (University of Arizona) and Gill Roper-Hall (Louisiana State University), plus Drs John Dickson (Waikato), Donny Suh (California), Wendy Marshman (Melbourne) and Andrea Molinari (Ecuador). This global powerhouse panel was chaired by Queensland’s Professor Shuan Dai.
Patients were brought onto the stage for assessment of their strabismus. This allowed the audience an up-close view of how these experts assess. My key learnings were:
- To always do a cover test in all positions of gaze, while carefully observing the patient for head movements as well as eye movements
- To repeat tests to ensure consistency of results
- To give clear instructions, ‘keep focused on the target’ or ‘make sure you are looking at the E’. The experts often clarified or repeated their instructions to ensure accuracy of their measurements
- When correcting for a compensatory head posture with prism, always correct over the dominant eye first.
This made me realise the basics never stop being important and even with all the expertise in the world, we still need excellent patient rapport and clinical communication to achieve accurate results.

Drs Jay South and Rebecca Findlay, Professor Shuan Dai, Associate Professor Joanna Black and Dr Samantha Simkin (author)
Then came the best part: world experts openly discussing their thoughts. They explained challenges, such as the limitations of their surgeries, or times they had not achieved the required results, such as a vertical deviation that was left under corrected. They listened to other perspectives, then changed their plans.
The humility of these experts and their willingness to collaborate on their patient management plans, some of which will be implemented following the conference, demonstrated the patient outcome was always the main goal. I aim to be like this in my discussion of cases with others: open to learning, open to hearing other ideas and open to sharing my successes and struggles.
Final thoughts
During this meeting of minds in Brisbane, I often found myself reflecting on the last time I was at the Brisbane Convention & Exhibition Centre. It was in 2014 for my first ever international conference as a graduate optometrist, when I could only dream of the things I could learn, the changes we could make and the future of being a paediatric optometrist. Had baby optometrist Samantha known she would one day be discussing future research and clinical opportunities with world leaders, let alone standing on stage and sharing her work with the world, she would have been in shock!
If all this has happened in the last 10 years, I cannot wait to see what another decade will do as we inspire others to collaborate on our goals and believe that things can always be better for paediatric eyecare around the globe.
Dr Samantha Simkin is a therapeutically qualified optometrist with a PhD in childhood visual impairment. She has multiple peer-reviewed publications and regularly speaks at conferences on paediatric optometry, myopia management, causes of visual impairment and management of low vision in children. She conducts research for Blind and Low Vision Education Network New Zealand and clinical work with Te Whatu Ora Taranaki and Judd Opticians.