Bright minds shine light on ocular therapeutics
Until invited to report on the Ocular Therapeutics Conference (OTC), I’d thought the acronym stood for ‘over the counter’. I wondered if I was being sent to report on the OTT advertising of a certain pharmacy chain. However, the OTC is the only New Zealand meeting focused entirely on ocular therapeutics, organised by the Buchanan Ocular Therapeutics Unit in the University of Auckland’s ophthalmology department.
The OTC was a full-day programme delivered by some of our brightest minds, reporting on their world-leading research and developments in treatments – and with scarcely a mention of AI! The day was divided into ‘What’s new’, ‘What’s hot’, ‘What’s boiling’ (inflammation) and ‘What difference have therapeutics made to clinical practice?’.
The bioengineered cornea
The first of the two keynotes was Professor Gerard Sutton, from the University of Sydney’s Save Sight Institute. His topic was ‘A bioengineered cornea, are we there yet?’ He began by sharing his commercial interest in two companies, which have attracted funding from the Australian Government, and reminded us of the global unmet need for corneal transplants to relieve corneal blindness. With 12.7 million people on transplant waiting lists, only 1 in 70 will get one, while 53% of the world’s inhabitants do not have access to corneal transplantation. Although prevention is key, the next issue is how to get corneas to those who need them, he said.
Corneal transplants have evolved over 200 years, so the procedure is good but not perfect, with problems such as immunorejection, suture-related issues, slow visual rehabilitation and poor results in high-risk patients requiring expensive quality control, said Prof Sutton.

Drs Jay Meyer, Sarah Hull, Jo Sims, Rachael Neiderer and guest speaker Prof Gerard Sutton
A successful experiment will not cure blindness – that requires commercialisation of products, which requires collaboration, he explained. He talked of one company whose product accelerated corneal re-epithelisation, which was well tolerated and showed no adverse events, with reduced stromal scarring after 30 days. Another study group is producing purified human collagen, which has transparency and can be injected into the eye. Yet another is working on single-layer endothelial cell transplants, while international consortium BIENCO (Bi-o-En-gineered Co-rnea) is producing two-layer, partial-thickness bioengineered cornea implants and is looking to produce a three-layer, full-thickness iteration.
Aurion BioTech (with major shareholder Alcon) states that its cell therapy has the potential to restore vision to millions of people suffering from corneal endothelial diseases, with one donor cornea serving 1,000 recipient eyes. Unfortunately, an intact Descemet’s membrane is required, therefore it is not yet suitable for problems such as Fuch’s dystrophy. The estimated costs per patient and regulatory costs are curbing the company’s claims, for now.
A bioengineered stroma is another mountain to scale, but the future of bioengineered corneas certainly looks promising. Though it’s difficult to manage different scientists from different institutions, Prof Sutton also acknowledged the input of so many colleagues and the strong relationship between Australia and New Zealand in ophthalmology and optometry.
Inflammatory retinal disorders
In the afternoon, Dr Jo Sims, the second keynote speaker, spoke of inflammatory retinal disorders and how factors, such as patient characteristics, can affect the differential diagnosis. Factors, such as cancer treatments or immunotherapy, autoimmune diseases or undetected infection, may affect the disease course and therefore it is necessary to delve into a patient’s medical history, she said, and note high-risk lifestyles before choosing a treatment pathway.
A poor response to steroid or autoimmune treatment in a compliant patient may throw up a flag to reconsider the chance of infection or be something else lurking in the background. Dr Sims gave the example of infliximab and adalimumab being contraindicated in people with multiple sclerosis. Other general health considerations include diabetes, which makes steroids more problematic, and depression/anxiety exacerbated by steroids or previous cancer history. Other considerations, such as childbearing age, alcohol intake and smoking, will influence medication choices and the overall outcome.

Dr Hussain Patel, Prof Jennifer Craig, Dr Mo Ziaei, Prof Ilva Rupenthal and Dr Simon Dean
Disease modifying anti-rheumatic drugs (DMARDS) can take up to three months to be fully effective but need careful pre-treatment screening and counselling, including screening for infections such as tuberculosis, hepatitis B or C, HIV and other viruses; baseline blood tests; vaccinations (no live vaccinations to be administered while on DMARDs); discussions about infection risks, family planning, and/or alcohol intake are necessary. Dr Sims also advised giving patients printed information to inform them without terrifying them.
Another special consideration is pregnancy. It appears that uveitis activity tends to increase during the first trimester of pregnancy then decreases during the second and third trimesters, generally resulting in an overall improvement. However, some studies show evidence of rebound activity post-partum, said Dr Sims.
The treatment algorithm is different in children as they tend to be more at risk from steroids, but consideration of amblyopia is always top of mind. The problem, said Dr Sims, is more often the decision about how to stop treatment rather than how to start it. Her advice is to aim for at least two to three years of steroid-free remission of uveitis before reducing DMARDS. Her take-home messages were:
- Consider the mechanism of retinal inflammation. Is it autoimmune or autoinflammatory versus infection versus masquerading?
- Tailor the treatment to the patient and the disease, aiming to preserve both vision and quality of life.
- There is a strong role for DMARDS in the management of chronic retinal inflammation.
- Don’t be too slow to phone another specialist for their opinion.
Microbes, mice and lethal lights
Professor Jennifer Craig presented on the recently released Tear Film & Ocular Surface Society Dry Eye Workshop (TFOS DEWS) III report for definition, classification, diagnosis and management of dry eye disease (DED). One of TFOS DEWS III main updates is the diagnostic screening tool, which teases out additional symptoms of tear-film markers or ocular surface markers. It also discusses symptom levels in those under 39 and recognises other ocular surface abnormalities, not just the tear film.
As interesting as Prof Craig’s presentation was, she was upstaged by her husband Dr Simon Dean’s arrival in a formal black tuxedo – minus the black bow tie – at 11.30am to present his novel UVC-emitting device, PhotonUVC. First, he tried to convince us that his attire was not a leftover from the previous night, but was in preparation for an imminent concert performance, playing double bass. Without taking a bow, he then launched into the history of light-based ocular therapeutics and his own history of building 12 crosslinking (CXL) machines (as one does), because they were not available in New Zealand, and finding that crosslinking can also be used to treat infections.

Khyati Jindal and Sarah Augenstein
Photoactivated chromophore for keratitis-CXL (PACK-CXL) is an exciting innovation intended to address the issue of antibiotics not keeping up with superbugs, as well as other issues with wrong choices, storage and supply, plastic waste and patient compliance.
Light therapy avoids some of these issues, said Dr Dean. UVA must get through the atmosphere to Earth’s surface but fails to kill off the nasties; UVB transmits a little through the atmosphere but is toxic to host cells, causing some cancers, though it has good antimicrobial effect after 10–20 minutes’ treatment. PACK-CXL requires the same treatment time but uses UVC, which does not penetrate the atmosphere naturally but can be emitted by LEDs in the specific wavelength that kills pretty much anything by going straight to the DNA of microbes. It reduces microbial load, killing bacteria, viruses, fungi, protozoa and moulds. Over-treating causes minimal cell damage, since DNA in a simple cell, such as a bacterium, breaks up more readily than in a mammal. It cannot entirely replace antibiotics but light therapy is non-invasive and avoids the delay using the wrong antibiotics, said Dr Dean.
The device is undergoing human trials to gain regulatory approval for use in New Zealand but it is already being used by UK vets as a quick (five seconds and no culture time) repeatable and painless standalone treatment or in conjunction with antibiotics.
Dr Rachael Niederer followed her first talk on anti-inflammatories and immunomodulators with a look at the microbiome and its place in eye disease. She stunned many of us by stating that babies born by Caesarean section are more prone to obesity, as well as increased risk of some mood and neurodevelopmental disorders.

Sponsor Optimed’s Robert Nyenkamp and Clarke Grieve
After introducing us to ‘bubble mice’, we started to wonder if we were in the wrong play group. However, it transpires that bubble mice are mice born by C section and raised in a sterile environment, meaning they have underdeveloped immune systems. This makes them very useful for studies of how the microbiome affects us, since the gut microbiome is now known to be associated with development of neurotransmitters including serotonin, dopamine and gamma-aminobutyric acid, which shapes mood. Around 90% of serotonin is made in the gut and the microbiome is also a major trainer of the immune system, shaping our immune function, said Dr Niederer.
The bubble mice are resistant to obesity, even when fed a high-fat diet, have altered stress responses and anxiety behaviours (gut-brain axis) and are less susceptible to autoimmune diseases but more susceptible to infections. They also metabolise drugs differently.
Ocular diseases associated with the microbiome are uveitis, AMD, diabetes and glaucoma. Gut-derived inflammatory signals and microbial metabolites promote neuro-inflammation, retinal ganglion cell death and disrupt the blood-retinal barrier, she said.
Probiotics are live organisms that alter the microbiome. In inflammatory bowel disease, probiotics have been shown to reduce disease flare-ups and severity. Prebiotics, meanwhile, are dietary components found in fibre-rich plant foods that support the growth of healthy bugs and suppress harmful ones.

Drs Jabelle Lu and Lucy Lu
Intermittent fasting has been shown to increase microbiome diversity and enriches beneficial organisms. This is associated with a reduction in pro-inflammatory cytokines and increased regulatory T cells. Unfortunately, when it comes to intermittent fasting, more is not necessarily better, with too much fasting increasing inflammation, said Dr Niederer.
Tears and the blinking menopause!
Hormones, particularly the problems they create when their levels alter drastically in the body, are a topic rarely discussed in polite company. Associate Professor Stuti Misra had no such qualms and encouraged us to approach our patients similarly, particularly when discussing DED treatment. The menstrual cycle, menopause and perimenopause all cause changes in oestrogen, which contributes to cognitive, gut, kidney, bone and cardiovascular health.
Oestrogen and progesterone are both present within the ocular surface and the tear film. During the menstrual cycle there is an increase in dry eye symptoms, inconsistent blinking patterns and reduced tear production, which manifest as ocular discomfort.

Celeste Raisbek, David Lee and Jane Patterson
Oral contraceptives interrupt the cycle and may cause insufficient tear production and increase DED symptoms, particularly in contact lens wearers. Increased exercise improves tear quality in the ovulation phase, while a sedentary lifestyle, particularly with poor sleep quality, disturbs the normal ocular surface.
After a question on whether the timing of refractive surgery to coincide with the menstrual cycle would be a good way to minimise DED issues post-surgery, session chair Dr Mo Ziaei brought this session to a rapid close.
The University of Auckland’s Dr Natalie Allen’s topic was corneal transplants, highlighting that the Covid-19 years saw a global reduction in donor corneas, partly thanks to the virus’ ability to survive up to seven days after the host’s death. The good news is that there was no significant difference in the initial visual outcomes of grafts during the Covid-19 years. However, there was a higher number of delayed clinical appointments corresponding to worse visual acuities one year post graft. A study of graft rejection at Auckland Public Hospital between 2010 and 2022 showed no statistical increase, said Dr Allen.
The effects of Covid-19 vaccines remain a big question. While it is likely that there may be a link between the vaccination and graft rejection, surprisingly the data seem to indicate a decreased risk, she said.
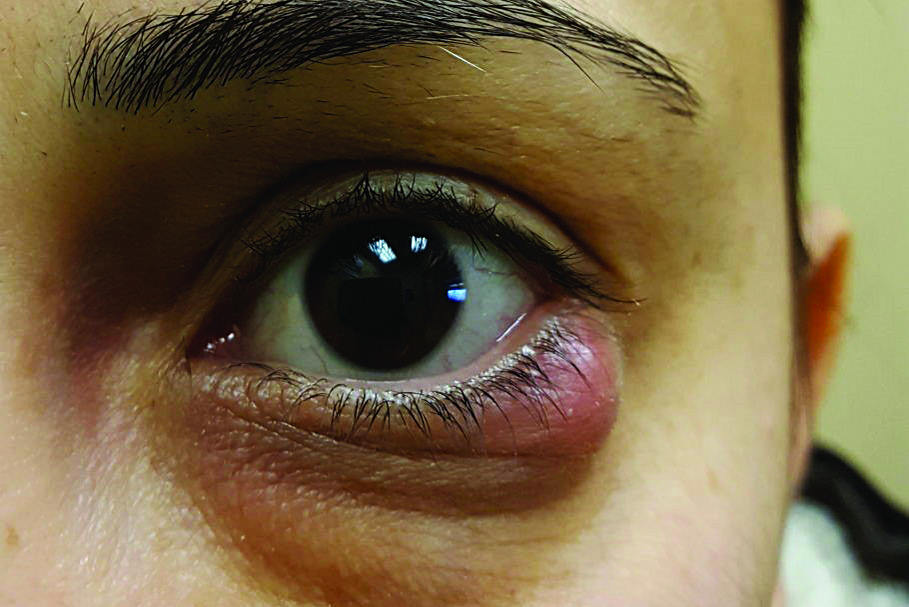
Armed with some new, local knowledge, Dr Jay Meyer discussed the features of allergic eye disease and his shock at encountering Auckland’s trifecta of pollen, wind and high humidity. After giving the pros and cons of various first-choice pharmacological and non-pharmacological treatments and their availability, he then discussed tacrolimus 0.1% ointment, which is an immunosuppressant and beneficial for inflammatory skin conditions such as eczema and psoriasis. It has a low systemic absorption, but he warned that it is not to be used during pregnancy and is only available at high cost on prescription, though it can be funded by special authority.
Vitamin D deficiency is linked with increased prevalence and severity of allergic conditions. Supplementation may reduce the severity in deficient patients but is not a substitute for standard therapies, said Dr Meyer.
The big surprise came under the heading of what not to prescribe. Lanolin, a component of sheep’s wool, was named 2023’s allergen of the year by the American Contact Dermatitis Society due to increasing allergic reactions. Lanolin is also present in Poly Visc and VitA-POS eye ointments. Judging by the gasps around the room, I was not the only one shocked by this. Perhaps our rural colleagues were less surprised. Given the number of New Zealanders who have direct daily contact with wool, 2–3% of population having a wool allergy is significant.
Drops, RCES and YAG
A good glaucoma-management tip from Dr Hussain Patel was to get patients to bring their eye drops with them to consultations. Almost every glaucoma patient has dry eye or ocular surface disease, which is often exacerbated by the preservatives in their glaucoma drops. Preservative-free glaucoma medications are available but the options are limited in New Zealand, have significant cost and there are significant variations across pharmacies, which do not always know of or have available preservative-free options and will often give the usual drops stacked with preservatives. So taking a look at what the patient is actually taking can be revealing.
Although 25–40% of recurrent corneal erosion syndrome (RCES) is caused by trauma, said Dr Sue Ormonde, many cases are triggered spontaneously, often due to corneal dystrophies such as Map-Dot-Fingerprint dystrophy (a useful descriptive term to explain to patients what you are seeing on the slit-lamp). She recommended using nightly ointment for two months to reduce recurrence, showing a slide of Poly Visc and VitA ointments – Dr Meyer’s wool allergy culprits! Dr Ormonde pointed out that patients often fail to use the ointment for the time they are directed to. She also advised us to get rid of Demodex mites, which are often present, and address any blepharitis.

Melinda Calderwood and Jordan Cooper
A novel treatment that requires more study is the use of insulin drops, which appear to be effective in improving the rate of epithelial healing. At present, this needs to be compounded by a pharmacy.
YAG laser can be used to create stromal micropuncture translucent scars that promote adhesion between basement membrane and epithelium. This appears to have some success in approximately 50% of cases. The ultimate paradox, according to Dr Ormonde, is that excimer laser both causes and cures RCES!
Inherited diseases, myopia and CXL
Children were not overlooked on the day either, with Dr Sarah Hull discussing therapeutics for childhood inherited diseases and outlining the many challenges in accurate diagnosis and time-sensitive new treatments, while Dr Rasha Altaie covered whether atropine slows the progression of myopia. She defined pre-myopia as a refractive state of an eye of less than or equal to +0.75D and greater than -0.50D in children, where a combination of baseline refraction, age and other quantifiable risk factors provide a sufficient likelihood of the future development of myopia to merit interventions.
This definition is useful in the discussion with parents and the many options for a preventative pathway, not forgetting the most important and readily available being time outside in the sun (or at least daylight, if sun is in short supply).
Dr Ziaei’s talk on corneal crosslinking (CXL) reminded us this is the only treatment to address the pathophysiology of keratoconus, espcially to stop progression. In a safe procedure, the endothelium must be left unharmed. Ultimately, the aim is to decrease treatment times and improve patient comfort by using higher intensity UV light, which gives improved visual outcomes. By pulsing the light, more oxygen is available, which improves the treatment.
CXL Plus is a combined treatment developed to simultaneously address disease progression and give better visual quality, but every treatment modality has potential complications. The future management of ectasia is almost certainly a combination of treatments, he said.
The OTC committee of Professors Ilva Rupenthal and Charles McGhee and Dr Trevor Gray delivered a full day of high-quality education. The only disappointment was the small turnout of registrants, with many of the mostly optometrist participants being from out of Auckland.

Naomi Meltzer is an optometrist who runs an independent practice specialising in low-vision consultancy. She is a regular contributor to NZ Optics.