Diagnosis and management of eyelid melanoma
Cutaneous melanoma is a life-threatening malignancy with a rising global incidence. Aotearoa has one of the highest rates of melanoma in the world.
Eyelid melanoma, while rare – accounting for less than 1% of all cutaneous melanomas – carries a better prognosis than on other parts of the body, especially those outside the head and neck region1. The better survival rate is partly due to early detection, facilitated by the high visibility of the eyelids. However, the prognosis worsens significantly in the presence of metastases, a risk facilitated by the rich lymphatic drainage of the head and neck. Additionally, the eyelids are closely related to the eye, posing a serious threat to visual function in the event of invasion, with the possibility of orbital exenteration.
These factors highlight the importance of recognising this entity and maintaining a low threshold for referral when evaluating suspicious eyelid lesions that could represent melanoma.
Clinical presentation
The majority of patients with melanoma present in their sixth or seventh decade. They may have a high number of freckles, a light complexion and a reaction to sun exposure characterised by burns without subsequent tanning. Eyelid melanomas are most frequently located on the lower eyelid, followed by the upper lid, lateral canthus and medial canthus. They mainly affect one side and rarely present bilaterally. Eyelid melanomas can rise from preexisting lesions or de novo.

A 74-year-old male referred for assessment of a pigmented lesion on his left lower eyelid and cheek. He’d had it most of his life and it had slowly changed in size and shape over the last 15 years. It was an irregular, ill defined superficial spreading melanoma which underwent excisional biopsy, margin control by frozen sections and reconstruction. During his six-month follow-up, there was no evidence of recurrence or metastases
The application of the ABCDEFG criteria is a valuable tool for identifying suspicious lesions2. Melanomas can be asymmetrical (A) in shape and/or colour. They often have ill-defined, irregular, and mixed sharp and fading borders (B). They are typically pigmented; a brown lesion is present in 96% of cases, but in 50% of cases they present as blue, black, tan, grey, pink or red. Apart from this colour variability with an irregular distribution, they can also exhibit colour changes (C). A pigmented lesion that is obviously different (D) from the others, a 'black sheep', must also be considered suspicious, even if it does not fulfil the rest of the ABCDEFG criteria. Melanomas can also evolve and change in size, shape or colour over time, or even present as a new elevated (E) or thickened lesion. Although firm (F) lesions can also be benign, as seen in a dermatofibroma, this feature can also be a characteristic of melanomas. Some forms can show rapid growth (G) with an increased size over weeks or even days. If advanced, they can present as an elevated, tender, itchy, bleeding and ulcerated area. Nevertheless, some melanomas may be dismissed as benign lesions (even skin tags) or other malignant tumours (such as squamous or basal cell carcinomas).
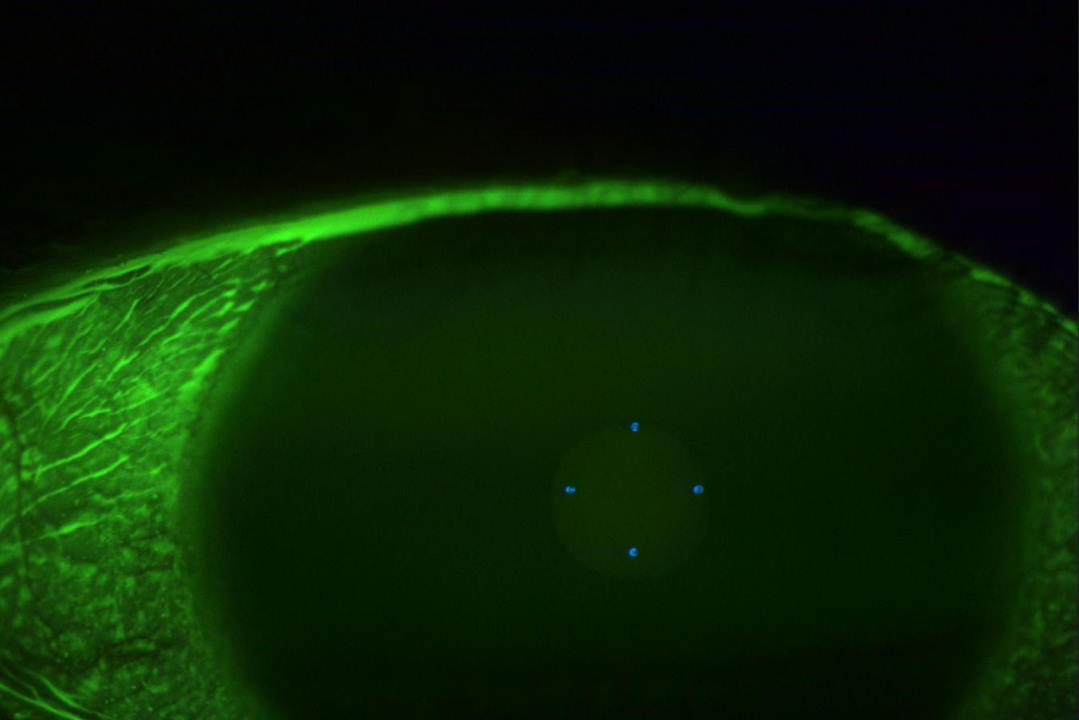
In such cases, it is essential to promptly refer to an oculoplastic specialist and to employ slit-lamp imaging or external photographs to monitor changes.
Management
Management must be individualised, frequently requiring complete excisional surgeries. The preoperative clinical assessment includes inspection and palpation of the eyelids and lymph nodes to assess for possible metastasis. In primary cutaneous melanomas, wide local excision with clinical excision margins of 1–2cm is the treatment of choice. However, these guidelines are difficult to follow in the periocular area without causing extensive functional impairment and cosmetic disfigurement due to the scarcity of eyelid tissue. The excisional biopsy requires ensuring clinically free margins for the melanoma and usually presents a reconstructive challenge. Orbital exenterations may be necessary if there is extensive infiltration of the eye and periocular tissues. In selected cases of melanoma, sentinel lymph node biopsy or locoregional lymph node dissection is indicated. Other treatments include immunotherapy, chemotherapy and radiotherapy. For all cases, multidisciplinary strategies are essential.
Prevention and education
There are multiple causes for cutaneous melanoma, with well-established risk factors such as solar radiation exposure, the presence of melanocytic naevi, family history and personal history of melanoma. Therefore, it is beneficial to advise all patients on sun protection, including the use of sunglasses that block 100% UVA/UVB, applying plenty of broad-spectrum, water-resistant sunscreen of at least SPF30, wearing long sleeves, walking in the shade, avoiding peak-sun hours and using broad-brimmed hats. Moreover, consider diet adjustments and encourage routine skin checks, especially in older, fair-skinned patients and those at higher risk of melanoma due to the presence of multiple naevi or prior skin cancers3.
Patients with a history of periocular melanoma need lifelong follow-up because local recurrence, regional metastasis and secondary neoplasms are not uncommon. Optometrists can support ongoing surveillance through routine external exams and prompt referral of any suspicious change.
Ultimately, awareness is key. Through collaboration between optometrists and oculoplastic surgeons, the early detection of periocular melanoma is not only possible but also sight- and lifesaving.
References
1. Dini F, Susini P, Zuccaro B, Nisi G, Cuomo R, Grimaldi L, Perillo G, Tinunin L, Antonini P, Innocenti A, Cecchi G, Gambale E, Doni L, Mazzini C, Santoro N, De Giorgi V. Head and neck melanoma: the eyelid region has a better prognosis and easier management. A retrospective survey and systematic review. Melanoma Res. 2024 Oct 1;34(5):429-438. doi: 10.1097/CMR.0000000000000984. Epub 2024 Jun 3. PMID: 38833343.
2. https://dermnetnz.org/topics/abcdes-of-melanoma
3. Watson AE, Yusuf N. The Influence of Dietary Factors on Melanoma Development and Progression: A Comprehensive Review. Nutrients. 2025 May 31;17(11):1891. doi: 10.3390/nu17111891. PMID: 40507159; PMCID: PMC12157913.

Dr Anna March de Ribot is a consultant ophthalmologist specialising in oculoplastics with a particular interest in clinical research. She’s based at Whangarei Hospital and collaborates with Te Whatu Ora Auckland.