Hot topics with Retina Specialists
Retina Specialists’ winter education evening is always a cosy affair that feels like you’ve been invited to dinner with friends, aside from the intriguing case deliberations that is!
First up was Associate Professor Andrea Vincent, who shared two case studies before a call from Starship prompted her early exit. Her first case, a middle-aged woman from the Cook Islands, had walked into the consult room with an unusually wide gait. A combination of pigmentary retinopathy, hearing loss (she had cochlear implants) and the obvious balance problem led her to suspect Usher syndrome. However, genetic testing showed the patient had a rare genetic disorder called PHARC (polyneuropathy, hearing loss, ataxia, retinitis pigmentosa and cataract) syndrome caused by mutations in the ABHD12 gene.
A more common presentation, A/Prof Vincent’s second case involved a young woman (aged 23 years) who had just recovered from Covid-19 and had been referred by her optometrist due to a sudden onset of floaters and what she thought was scotoma around her peripheral vision. Infrared imaging showed some disruption of the macula and some darkening, while multifocal electroretinography confirmed there was a corresponding area of attenuation in the right eye while the left eye wasn’t quite as marked but similarly showed a slight reduction just nasal to the fovea.
With genetic testing inconclusive, A/Prof Vincent decided to review the patient in 12 months. At that point, the woman’s vision was pretty much unchanged. Comparing infrared imaging of the macula with the previous imaging, she noted that, while there was still disruption, the darker areas had definitely faded. Repeating the electrophysiology, it revealed an improvement, implying there had been a vascular event, possibly associated with the Covid-19 infection.
Increasingly, the literature is finding vascular events can occur in the retina in connection with Covid-19, including cotton-wool spots and retinal microhaemorrhages, she said. Covid-19 has also been associated with new-onset paracentral acute middle maculopathy and acute macular neuroretinopathy, although a definitive relationship between these conditions and Covid-19 is yet to be established, A/Prof Vincent concluded.
Lucky escape

Retina Specialists' new ophthalmic nurse Miriam Petterson, Sasha O'Sullivan, Anna Maitland and Michael Yip
Impressed by the ophthalmic knowledge in the room, Dr Rachel Barnes quizzed optometrists on the potential diagnoses and investigative techniques for three cases involving ocular ischaemic syndrome, lupus and myelinated nerve fibres.
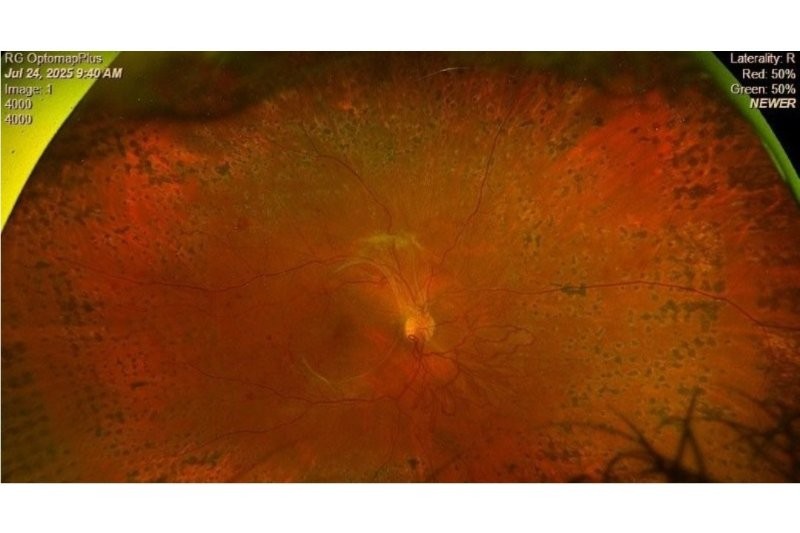
Referred by his optometrist, the ‘lucky escape’ was a 59-year-old male who presented with spotted retinal haemorrhages during a routine eye examination. Imaging revealed scattered block haemorrhages and engorged-looking veins in the right eye, while the left eye looked normal. He had slightly blurry vision in the right eye, normal anterior segment and no significant cataract. Having checked the venous pressure wasn’t raised, Dr Barnes said she listened to the carotids and could hear a bruit (a sort of turbulent flow synchronised with the heartbeat) on the left side, while the affected right side was pretty quiet. Suspecting ocular ischaemic syndrome, Dr Barnes ordered a carotid ultrasound.
The result was alarming: severe plaques in both common carotid arteries, severe plaques at the origin of both internal carotids, 80–99% stenosis of the right proximal internal carotid artery and 70–79% stenosis of the internal carotid artery and both external carotid arteries. “He was a walking time bomb,” Dr Barnes said, adding there was so little flow on the right, affected side you couldn't even hear the bruit.
The man was urgently referred to vascular surgeons and had an endarterectomy on his right side within days and the left one done about four weeks later. Seeing Dr Barnes some days after his second endarterectomy, the patient said he was feeling so much better and clearer in the head. “Turns out it's quite good to have blood going to your brain!” she said.
AI in practice
Dr Leo Sheck piqued optometrists’ interest with talk on the use of artificial intelligence (AI) in practice. Sharing a case of hydroxychloroquine retinal toxicity, he said a newly developed open-source AI tool called HCQquery can detect the presence of hydroxychloroquine retinopathy and predict its future occurrence from spectral-domain OCT (SD-OCT) images. Dr Sheck said the algorithm achieves excellent performance metrics, with an accuracy of 0.987, sensitivity of 1.00 and specificity of 0.983. He said it’s important to note these tools are unregulated, so they can only be used in a research setting.
“Ultimately, you need to make your own clinical decision. What I do is that I only use the algorithm at the end for verification, having formulated my diagnosis first,” Dr Sheck said. “Because, little by little, like seeing other people's choices on the screen when doing quizzes, it will influence what you choose. Seeing a result from a deep-learning algorithm will influence how I interpret the scan, so it’s really important that you do everything yourself first and then maybe run the algorithm on the imaging just to confirm what you concluded from the imaging.”
Hope on the horizon
Wen Li, Jacqueline Ling and Christina Herrick
Having recently returned from the American Society of Retina Specialists’ annual meeting, Dr Sheck said there was a lot of discussion on management of geographic atrophy and intermediate AMD. He said there is something good on the horizon for these patients, beyond the Amsler grid and supplements: photobiomodulation (PBM). LumiThera’s Valeda Light Delivery System was approved by the FDA late last year and Dr Sheck said he anticipates it will be available in New Zealand next year, now Alcon has acquired the company.
PBM is a non-invasive treatment using low-level light therapy in three distinct wavelengths of yellow, red and near-infrared radiation to stimulate mitochondrial energy production, promoting retinal cellular health. It’s administered to the patient while they sit comfortably in a chair, and they come in for nine sessions over three to five weeks, have a break for four months, then return and do it again. Trials have shown the treatment improves visual acuity; however, more interestingly, the macular drusen volume decreased following treatment, Dr Sheck said. “That's probably more convincing, people who have been treated have got less drusen. Still, a decrease in volume of drusen may not always be a good thing, as they sometimes collapse and leave behind atrophy. But what they've shown in this study is people who have been treated with photobiomodulation have less incidence of new-onset geographic atrophy as well, so that is looking quite encouraging.”
On that positive note, Retina Specialists wrapped up another successful education evening.
HCQuery is available here The algorithm will accept OCT images in png, tiff or jpg formats.