Rare report of orbital pyoderma gangrenosum
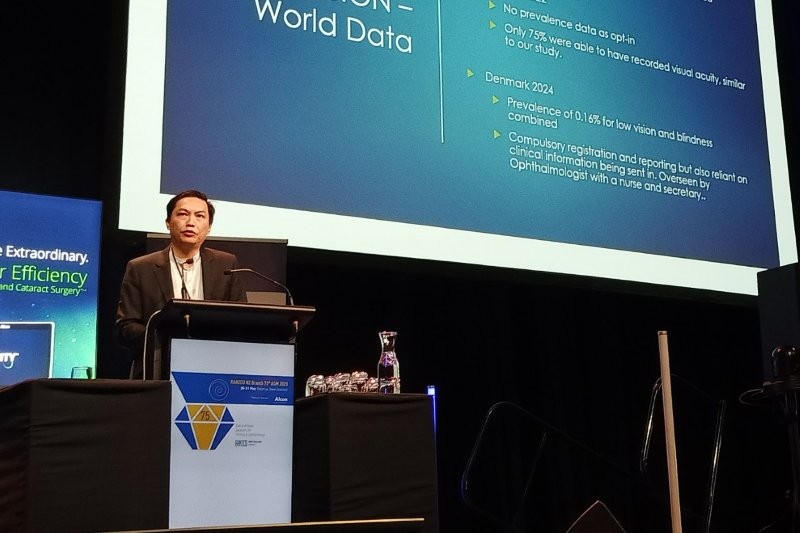
A rare and grisly case of the autoimmune condition pyoderma gangrenosum (PG) was documented by Nelson Hospital’s Drs Garry Singh and Sacha Moore, and presented as a poster at the RANZCO NZ 2025.
The doctors’ account said the worldwide incidence of PG is estimated to be three to 10 cases per million population per year.
Initially assumed to be an abscess, a painful unilateral orbital swelling had developed rapidly over five days in a 77-year-old man. Following referral from his GP, it was ascertained at Nelson ophthalmology clinic that he also had a recent ulcerated left leg infection and left fifth digit swelling, which was being treated with oral flucloxacillin. Despite generalised malaise, he had no fever and reported no pain on eye movement, eye redness, eye pain, light sensitivity or blurring.
Viral and bacterial swabs returned negative results and attempted drainage of the lesion produced no pus. Bloodwork showed an elevated white cell count, with neutrophilic predominance and highly elevated C-reactive protein levels. Although punch biopsies showed acute inflammation with debris, they were considered non-diagnostic. An urgent CT scan showed a large solitary mass on the left orbit, not typical of a drainable abscess or invasive malignancy.
Following referral to dermatologists, a diagnosis of PG was made, with probable superimposed bacterial infection. After four weeks of tapering prednisone (40mg daily for seven days and subsequent 10mg reduction per week), continued oral antibiotics, daily 10-minute vinegar soaks, plus topical paraffin 50/50 and triamcinolone treatment, complete resolution of the lesion was achieved.

Left periorbital lesion resolved at
four-week follow-up
The doctors concluded that clinicians should consider PG as a differential diagnosis if patients present with rapidly progressive lesions with atypical features. There is no definite diagnostic test for PG, so work-up should include a blood panel, cultures of affected sites, biopsies for histology and orbital imaging. Recurrence is not uncommon, and corticosteroids are the mainstay of treatment alongside supportive measures, they said.