Semaglutide and ocular health
The recent arrival of synthetic incretins (gut-derived hormones secreted after eating, which stimulate a decrease in blood glucose) onto the market has led to an explosion in their use, primarily for weight loss and as an adjunct in diabetes control. Fuelled by celebrity endorsements, semaglutide (glucagon-like peptide-1 receptor agonist, sold as Ozempic or Wegovy) became the most prescribed drug in the US in 2023. As a result of widespread use, its effect on ocular health is becoming more defined and is beginning to be discussed in the literature.
Risk of NAION in patients prescribed semaglutide
Hathaway JT et al.
JAMA Ophthalmol. 2024: 142(8):732-739.
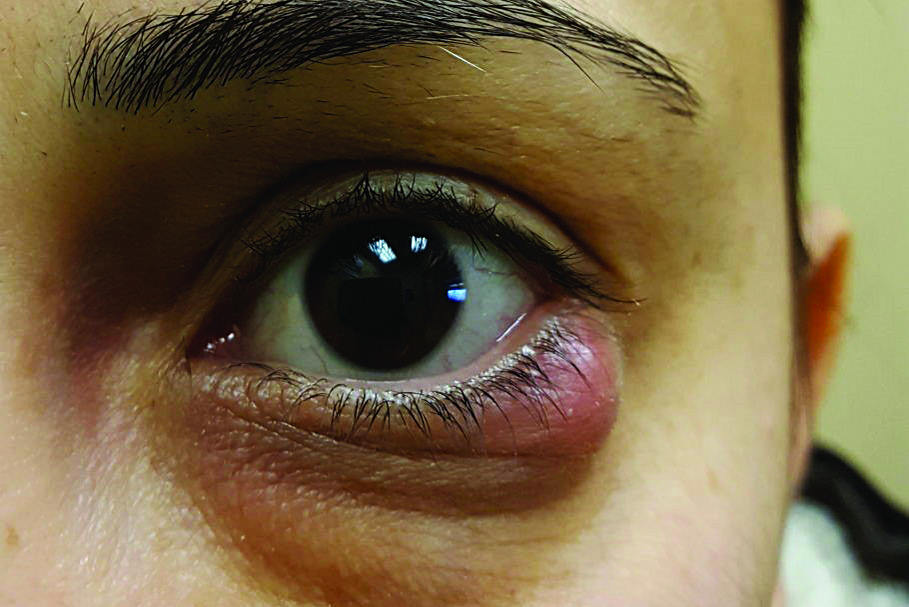
Review: This retrospective matched cohort study looked at 16,827 patients seen in the neuro-ophthalmology clinic at Massachusetts Eye and Ear between December 2017 and November 2023. It identified 710 patients with diabetes, 194 of whom were exposed to semaglutide and 516 who were not. In the semaglutide group 8.9% developed nonarteritic anterior ischaemic optic neuropathy (NAION) compared to 1.8% in the non-semaglutide cohort. The study further identified 979 patients who were overweight or obese, in whom 361 were exposed to semaglutide and 618 who were not. In the semaglutide group 6.7% developed NAION compared to 0.8% in the non-semaglutide group. Thus, patients with diabetes were over four times more likely to develop NAION if they were taking semaglutide, compared to controls, and eight times more likely if overweight or obese.
Comment: This was the first study to report an association between semaglutide and NAION. Given the high demand for the medication and its substantial benefit in controlling type 2 diabetes and efficacy in achieving a significant weight loss for the patients, it is prudent to be familiar with the possible link between semaglutide and this potentially devastating ocular complication.
Are synthetic incretins associated with ischaemic optic neuropathy?
Gregory V, Mollan SP
Eye; Feb 2025
Review: This editorial summarises a handful of available studies on the possible association between semaglutide and NAION. Some show an increased risk of developing NAION either within first 12 months of beginning semaglutide treatment or during five years of treatment, while others do not show any increase in risk. Of particular interest is the note saying it’s unfeasible to conduct an ophthalmologic examination to detect the presence of ‘disc-at-risk’ prior to starting semaglutide. This is due to the large number of patients involved and one of the studies suggesting that absence of a cup may be less relevant for such patients. It was suggested that patients with a history of NAION, vision loss from previous optic neuropathy or optic disc drusen may require ophthalmological assessment and shared decision-making in regard to risk-benefit ratio of initiating semaglutide therapy.
Comment: As the number of patients on semaglutide is only going to increase, it pays to be familiar with controversy in the literature on the possible increased risk of NAION. This would need to be weighed carefully against the benefits of improvement in diabetes control and achievement of significant weight loss.
The effect of GLP-1RA exenatide on idiopathic intracranial hypertension
Mitchell JL
Brain 2023:146; 1821-1830.
Review: This randomised, placebo-controlled, double-blind trial assessed the effect of the glucagon-like peptide-1 (GLP-1) receptor agonist exenatide (synthetic incretin) on intracranial pressure in idiopathic intracranial hypertension (IIH). Intracranial pressure was measured in 15 women (seven in the exenatide group and eight in the placebo group) with proven IIH (intracranial pressure >25 cm of cerebrospinal fluid (cmCSF) and papilloedema) at 2.5h, 24h and 12 weeks after initiation of treatment by means of telemetric catheter placed via 4mm burr hole into the right frontal lobe. Exenatide resulted in a statistically significant reduction of intracranial pressure at all study time points compared to placebo (0-5.7 cmCSF at 2.5 hrs, -6.4 cmCSF at 24hrs and -5.6 cmCSF at 12 weeks).
Comment: The study shows the potential for GLP-1 receptor agonists as a novel treatment of IIH. An interesting point is the rapid onset of intracranial pressure reduction at 2.5h after administration, which is particularly useful in cases of fulminant IIH, when rapid reduction of intracranial pressure is required to salvage remaining vision. The study is small but demonstrated a promising result.

Dr Taras Papchenko is a consultant ophthalmologist at Auckland Eye and Greenlane Clinical Centre, with sub-specialties in oculoplastics and neuro-ophthalmology. He graduated from Auckland Medical School in 2002 and was awarded a PhD in ophthalmology in 2013.