Anti-presbyopia drops – fact or fiction?
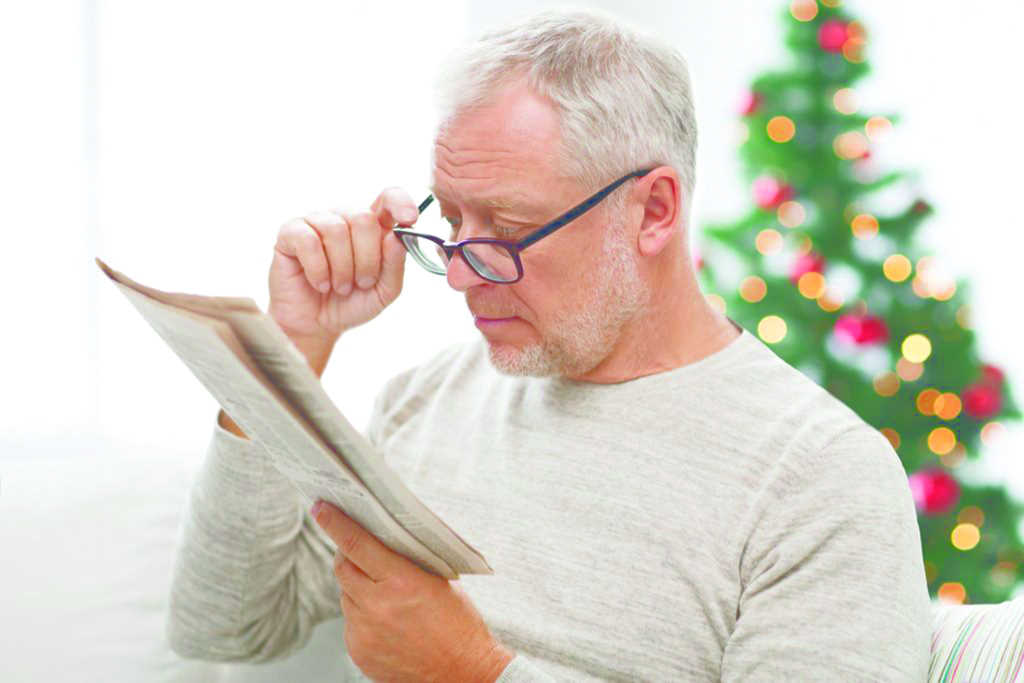
Presbyopia is almost as inevitable as death and taxes. Practical solutions have been sought since time immemorial, particularly ones that free us of pesky spectacles or contact lenses.
Such optical hardware and pinhole devices have been supplemented by pseudo-optical, mainly surgical, solutions such as the Crystalens intraocular lens (B&L) or a corneal implant such as the Kamra (SightLife Surgical), a pinhole aperture implant. The Presbyopic Allogenic Refractive Lenticule (PEARL) uses femtosecond laser monocularly to create a lenticule in the corneal stroma which then uses the patient’s own tissue for the presbyopic inlay. The result is modified monovision.
Dr Dean Corbett, an Auckland ophthalmologist with a keen interest in innovative solutions for presbyopia, said his preferred option depends on the patient and their appetite for surgical intervention. But only after they are fully informed about their visual development through early presbyopia, expression of latent hypermetropia and refractive and visual quality changes due to progressing changes in their crystalline lens. “I start with monovision contact lens simulations, then on to surgical lens replacement with a variety of intraocular lens (IOL) options,” he said.
Dr Corbett has not seen an increase in requests for spectacle-free presbyopia options since mask wearing became an everyday phenomenon, he said, but he’s aware of this trend overseas, which may relate more to mask wearing being compulsory.
Pharmaco-refractive treatments
The new remedy on the block is pharmaco-refractive treatment, with a plethora of chemical contenders throwing their hats into the ring. There are two broad categories for pharmaceutical correction of presbyopia, the first being the products that use pharmaceuticals to produce an optical phenomenon, such as the pinhole effect, to increase depth of field using miotics in combination with other known drugs. The miotic pilocarpine has known possible side effects including headaches and redness plus ciliary spasm, brow ache and even uveitis. Its effectiveness may vary with factors such as iris colour. To counteract such effects, most formulations have combined the miotic with other agents to reduce ciliary muscle contractions, inflammation, redness and discomfort.
The second group focuses on the root cause of presbyopia – the ageing of the accommodative system, thought to be the result of hardening of the crystalline lens and weakening of the lenticular fibres. These treatments actually change the composition of the lens and/or the lenticular zonules.
The first group is touted as the frontrunner and may be commercially available within one to three years. But to be successful, the finished product needs to:
- Be safe to use
- Show a measurable improvement – most studies report a number of lines or letters of improvement, which is often reported as distance-corrected near-vision acuity (DCNVA). It remains to be seen how this theoretical measurement of success relates to functional real-world near acuity and comfort
- Not compromise distance vision
- Demonstrate improvement in both photopic and mesopic conditions
- Sustain the effect over a number of hours
- Show minimal or no side effects - some anti-presbyopia drops may be available in preservative-free formulations, which would suit patients with pre-existing ocular surface disease
Other considerations include time to onset of action and maintaining the correct dosage, the latter being an issue with any topically applied therapeutic. Patients struggle with this even when the dosage is specified, as, for example, with glaucoma medications. Is there a risk if patients self-medicate on the assumption that if one drop is good, would two or three drops be better?
Crossing the FDA-approval finish line first in the presbyopia drops race is Allergan (AbbVie) with Vuity (previously AGN-190584), a single-agent drop containing pilocarpine 1.25%. The company reported in July this year that AGN-190584 had met its primary endpoint of greater than or equal to three lines of near and intermediate vision in mesopic conditions in the majority of presbyopic patients in its phase 3 clinical study, without the loss of distance acuity. There were no serious adverse events reported, with headache occurring in less than 5% of participants; and only 1.2% of patients discontinuing treatment. The drops acted within 15 minutes and their effects lasted up to six hours. Vuity was approved on 29 October 2021, making it the first and so far only FDA-approved eye drop to treat presbyopia, but its competitors are close behind.
Nyxol (Ocuphire Pharma) and VTI-001 Brimochol (Visus Therapeutics) are both combination agents, with Ocuphire combining pilocarpine and phentolamine, whereas Visus uses carbachol and brimonidine in its once-a-day formula to constrict the iris sphincter and inhibit iris dilator contraction. The latter product has the advantage of taking effect within 30 minutes and can last 8-10 hours.
Nyxol is reported to effect a decrease in pupil size of around 30%, lasting up to 15 days in almost 60% of the subjects under both photopic and mesopic conditions. The product uses a two-part regimen of phentolamine mesylate given at bedtime to reduce hyperaemia, and a low dose pilocarpine given the following day or days later, as needed. This is where the previously mentioned patient compliance and understanding may be an issue. Both Nyxol and VTI-001 are in phase 2 trials.
Eyenovia has a novel delivery method for its proprietary pilocarpine formulation, MicroLine, another single-agent pupil modulator. This is administered via the company’s Optejet device, which delivers the precise solution of pilocarpine in a mist to distribute the dose evenly over the cornea. The effect lasts three to four hours and is currently in phase 3 development.
CSF-1 PresbiDrops (Orasis Pharmaceuticals) is also in phase 3 trials. It combines an oil-based formula of mainly pilocarpine with a non-steroidal anti-inflammatory to reduce side effects. Novartis has taken a new direction with UNR844, which works on the premise that presbyopic changes in the lens and ciliary muscle are thought to be due to an increase in disulfide content. UNR844 penetrates the cornea, where it is metabolised into choline and R-lipoic acid. Enzymes within the lens break down the lipoic acid to the active form DHLA (dihydrolipoic acid), which breaks disulfide bonds, allowing greater elasticity in the lens. The most common adverse events were dysgeusia (altered sense of taste) and headaches in 5% and 3% of treated participants, respectively.
|
Company |
Product |
Mechanism |
FDA status |
|
Allergan |
Vuity |
Miotic |
FDA approved (29/10/2021) for daily |
|
Eyenovia |
MicroLine |
Miotic |
First Phase 3 complete |
|
Orasis |
CSF-1 |
Miotic |
Phase 3 initiated |
|
Presbyopia Therapies |
LiquidVision |
Miotic |
Phase 2b complete |
|
Visus Therapeutics |
Brimochol |
Miotic |
Phase 2 initiated |
|
Novartis |
Dioptin |
Lens |
Phase 2b planned |
|
Ocuphire Pharma |
Nyxol + Low-Dose Pilocarpine |
Miotic |
Phase 2 enrollment complete |
|
Viewpoint |
VP1-001 |
Lens |
Pre-clinical investigation |
|
OSRX |
EyeFocus |
Miotic |
N/A |
Table 1: the presbyopia drops pipeline
Prevention, not cure
Since the trials are attempting to reverse presbyopic lens changes, it seems likely that such products could be used in younger patients to delay the onset of presbyopia. This would increase the timeline over which proof of safety is a concern, which compares with miotic drugs which have an established history. Obviously, this option is not available to pseudophakes.
Alyssa Lie, research fellow and lecturer at the School of Optometry and Vision Science at the University of Auckland, has recently completed her doctorate research on the use of magnetic resonance imaging (MRI) to identify physiological biomarkers to predict the onset of presbyopia and age-related cataract. Her post-doctoral research involves going further down this line of investigation, so no doubt we will hear more of this topic in the future. Her aim is to use these biomarkers to inform the development of pharmaceutical agents that target the enhancement of the lens physiology for both presbyopia and cataract, which can then be tested using the MRI protocols established in the prior research.
There appears to be general agreement that the downside to the use of anti-presbyopia eye drops is the unknown risk of long-term use, with clinical trials not lasting long enough to ascertain what could arise after years of use. Given that once presbyopia arrives it settles in for life, this information is important.
Requiem for ready readers?
As to the question about the effects of these advancements on the optometry profession, Alyssa Lie said, “At first glance it may come across as a significant disruption to the optometry industry’s ‘bread and butter’. However, in reality it is unlikely to replace conventional treatment with optical correction (at least with the drugs that are going to hit the market soon). In my opinion, it would actually have an overall positive impact on the industry, as it gives us the opportunity to offer patients a novel solution to the age-old problem of presbyopia. Patients will be excited to know that their optometrists are keeping up with the latest medical advances, and it will increase public awareness about our therapeutic prescribing knowledge and capabilities.”
The anti-presbyopia drugs will be introduced into the pharmacology curriculum for optometry students, pending completion of phase 3 trials and FDA approval, said Alyssa. “As long as these anti-presbyopia drops are prescription only and not available over the counter, it would also be a great way to retain patients as they get older and are at higher risk of developing other eye diseases.”
Before long, we may be in a position to offer a range of pharmaceutical options. Patients will need proper instruction about whether they will encounter dark conditions, whether they need a full work day and when to consider monovision or binocular requirements, as well as potential side-effects and short- or long-term risks. They will, of course, still need that backup pair of spectacles.
Will the near future bring the ultimate in vanity: eyelash-lengthening mascara containing prostaglandins combined with miotic drops for presbyopia? In times to come, will we witness a line of youthful-looking millennials with lush eyelashes and saggy hypotonic eyeballs beating a path through the practice doors? Who knows, but with current developments, the future of presbyopia treatments is certainly looking brighter.

Naomi Meltzer has worked in optometry for more than 30 years and runs an independent optometry practice in Auckland, specialising in low vision consultancy. She is a regular contributor to NZ Optics.