Oh no, the drain is blocked! PXF and glaucoma
Pseudoexfoliation syndrome (PXF) is important to identify as it carries a significant risk of glaucoma. Once pseudoexfoliative glaucoma develops, it may run an aggressive course requiring close monitoring and intensive treatment to prevent significant visual loss.
Variants in the lysyl oxidase-like 1 (LOXL1) gene have been implicated as a major risk factor, increasing the risk of PXF – where a flaky substance accumulates on structures in the eye – by up to 20 times. The LOXL1 gene encodes for an enzyme important in the processing of some extracellular matrix components. The exact mechanism is still unclear, but it leads to progressive expression of PXF material from the anterior lens capsule, which then causes blockage of the trabecular meshwork. This reaches a critical point where the outflow facility is overwhelmed and intraocular pressure (IOP) rises. It is also associated with a higher risk of certain cardiovascular disorders, as the abnormal gene affects other organ systems.
Risk factors for PXF include Scandinavian or Northern European ancestry, but it can be seen in all races. PXF incidence increases with age, typically presenting in patients in their 60s.
Signs of pseudoexfoliation
It is a common cause of significant IOP asymmetry in patients over 60 years old. Other signs may be quite asymmetrical or even completely absent in the fellow eye.
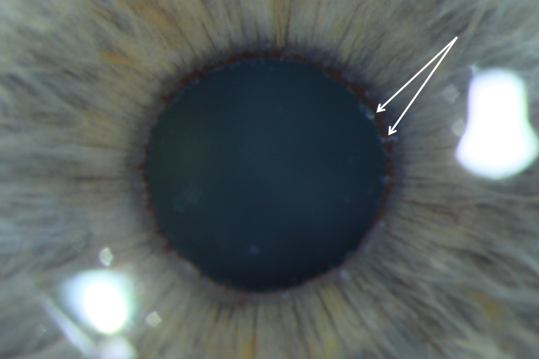
The classic finding is of fibrillar white material on the anterior lens capsule in a ring-like pattern (Fig 1a). This may best be seen with transillumination of the lens. Dilation will make the lens deposits more obvious (it may be missed in about 20% without dilation). In the condition’s later stages, pharmacological dilation may be limited due to deposition of PXF material in the iris. The pupillary margin ruff may also have the fibrillar material or look atrophic or absent (Fig 1b).
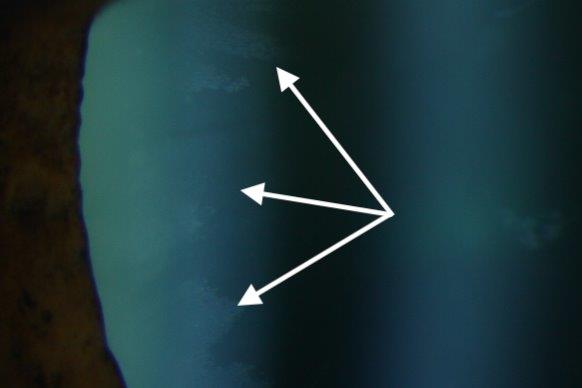
Fig 1a. Pseudoexfoliative material on the anterior lens capsule
It is important to compare the pupil margin tissues with the other side as this may be the only clue in early PXF. In advanced cases there may be phakodonesis or a shallow anterior chamber due to associated zonular laxity, which puts patients at higher risk of angle closure disease.
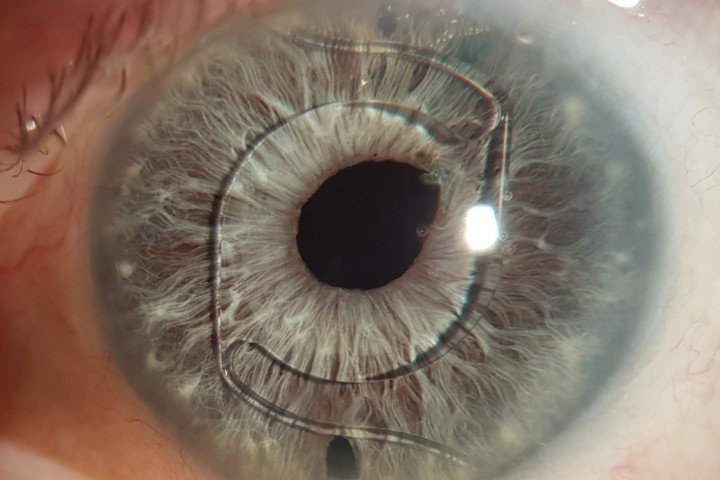
Gonioscopy shows a Sampaolesi line – pigment anterior to the trabecular meshwork (Fig 2). Transillumination of the iris may occur but this is more central than seen in pigment dispersion syndrome. Patients may present with advanced glaucomatous optic disc cupping and significant visual field loss.
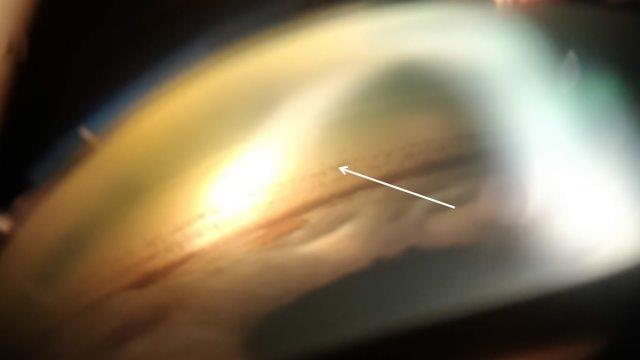
Fig 2. Sampaolesi line seen as a wavy line of pigment anterior to the trabecular meshwork
Glaucoma risk with PXF
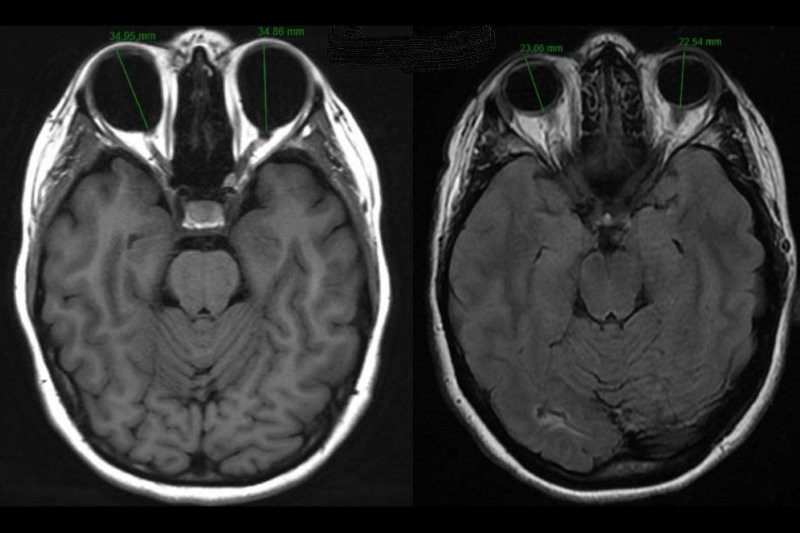
At least 50% of patients with PXF develop glaucoma and they may have higher and more labile IOPs compared to primary open-angle glaucoma (POAG) (Fig 3). It was the strongest risk factor for long-term progression identified in patients in the Early Manifest Glaucoma Trial.

Fig 3. OCT scans showing marked reduction in RNFL thickness over two years (left 2014,
right 2016) showing conversion from PXF with OHT to pseudoexfoliative glaucoma
Treatment
Drop treatment is usually the first line, but follow-up intervals may need to be shorter and there should be a low threshold for intensifying treatment. Selective laser trabeculoplasty (SLT) can be used to reduce the pressure, but clinicians need to be aware of possible post-laser pressure spikes and the risk of sustained high pressure requiring surgical treatment. As with drop treatment, follow-up intervals after laser should also be shorter than in POAG.
Trabeculectomy has been the mainstay of surgical treatment for many years but newer minimally invasive glaucoma surgeries (MIGS) such as Xen or iStent may allow faster visual recovery and have a better risk profile.
When there is co-existing cataract
Patients with PXF have a higher incidence of nuclear sclerosis. Cataract surgery in these patients can be challenging as they may dilate poorly, have weak zonules and shallow anterior chambers. Extra care must therefore be taken to reduce the risk of complications. Historically, these risks meant cataracts were often left until mature before being operated on, making the surgery even harder. Modern techniques for managing small pupils and weak zonules have changed many surgeons’ approach, so cataract surgery may be offered earlier, while dilation is still good and zonules are stronger. Cataract surgery alone may reduce pressure but there is a significant risk of early post-operative pressure spikes. They may also have more post-operative inflammation.
If there is need for both IOP control and improved vision, cataract surgery may be combined with glaucoma surgery such as Xen or iStent.
References
- Pasutto F, Zenkel M, Hoja U et al. Pseudoexfoliation syndrome-associated genetic variants affect transcription factor binding and alternative splicing of LOXL1. Nat Commun 8, 15466 (2017)
- Leske MC, Heijl A, Hyman L, Bengtsson B, Dong L, Yang Z; EMGT Group. Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology 2007. Nov;114(11): 1965-72

Dr Graham Reeves is a consultant ophthalmologist specialising in cataract and glaucoma for Counties Manukau Health and Eye Institute.