GNZ’s lessons in drop adherence
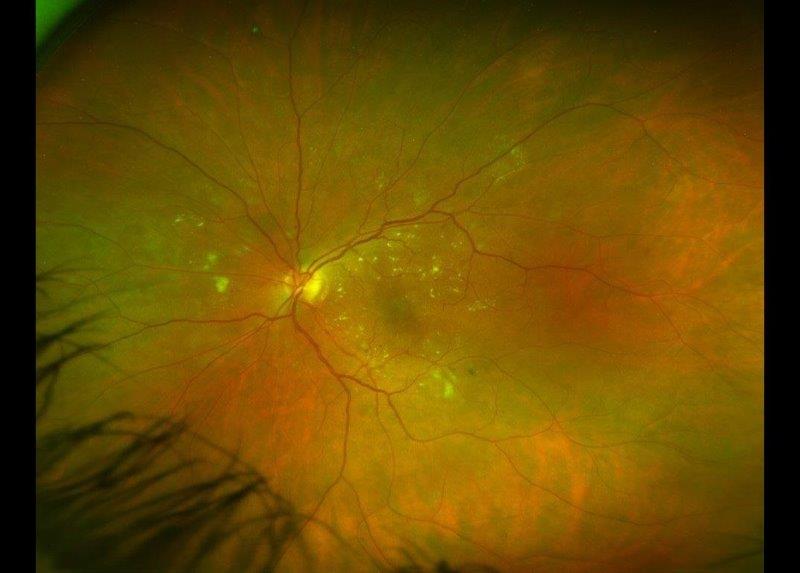
Glaucoma poses a significant threat to vision if left untreated. With 112 million people estimated to be affected by 20401, it ranks globally as the second leading cause of blindness2, emphasising the essential role of adherence to ocular hypertensive medications in preventing irreversible vision loss. However, patient adherence remains a persistent challenge, particularly among individuals facing chronic, asymptomatic conditions like glaucoma, where a lifelong commitment to treatment is necessary.
The World Health Organization recognises non-adherence as a complex behavioural process involving various factors3. Firstly, situational or environmental factors, including ongoing life stressors, co-morbidities and disruptions to routines, such as travel. Secondly, medication regimen factors, including the complexity of the medication regimen, cost and side effects. Thirdly, patient factors including forgetfulness, difficulties in medication administration (especially in elderly patients) and limited knowledge, impacting personal motivation to adhere. Fourthly, provider factors include dissatisfaction with care, miscommunication and specific communication barriers, such as inadequate time with doctors and limited understanding of medication benefits4. Challenges related to accessing appointments or pharmacies also fall under provider factors. Socioeconomic status, education level and support systems further influence adherence rates, with forgetfulness consistently emerging as a primary cause in numerous studies5,6.
In this context, education emerges as a fundamental approach to enhance knowledge and health behaviours, playing an integral role in addressing non-adherence in conjunction with effective communication.
Learnings from Aotearoa
A study conducted in New Zealand revealed significant misconceptions and knowledge gaps among glaucoma patients, notably the belief that they could rely on symptoms to gauge the deterioration of their glaucoma7. While numerous studies have investigated various communication methods and educational interventions to improve medication adherence, no singularly superior educational intervention has emerged to date. Instead, more effective strategies involved a multifaceted approach integrating multimedia education, written information, telephone calls and reminder systems8,9. The key emphasis lies in tailoring these approaches to each patient’s needs and barriers10.
Methodology
To gain deeper insight into the unique challenges faced by glaucoma patients in New Zealand, we initiated a small-scale pilot study via a telephone survey. The standardised survey gathered information from 90 individuals newly enrolled with Glaucoma New Zealand (GNZ). It included questions about how they were diagnosed, the timing of their diagnosis, any family history, their initial and current knowledge of the condition, their awareness of the complications associated with non-adherence, instances of missed eye drops in the last month, the frequency and reason for missed doses, current and past treatment, their relationship with their ophthalmologist and any difficulties faced in accessing appointments or medications.
These calls served as an opportunity to not only collect information but correct any misconceptions patients had through a more personalised approach. Such information was valuable for obtaining a clearer understanding of our patients’ needs, enabling GNZ to implement appropriate interventions and better support patients.
Results
The survey uncovered several key insights. Prior to their diagnosis, 21.4% of patients were unaware of glaucoma, suggesting the need to increase public awareness. Furthermore, 66.3% of patients were not familiar with their specific glaucoma subtype, suggesting the need for clearer communication and education initiatives. Encouragingly, 86.7% of patients consistently remembered to complete their eye drop regimen, alleviating concerns about forgetfulness. While 79% of patients expressed satisfaction with the amount of time spent with their ophthalmologist, a notable 32.2% desired more comprehensive information about their condition and management options from their ophthalmologist.
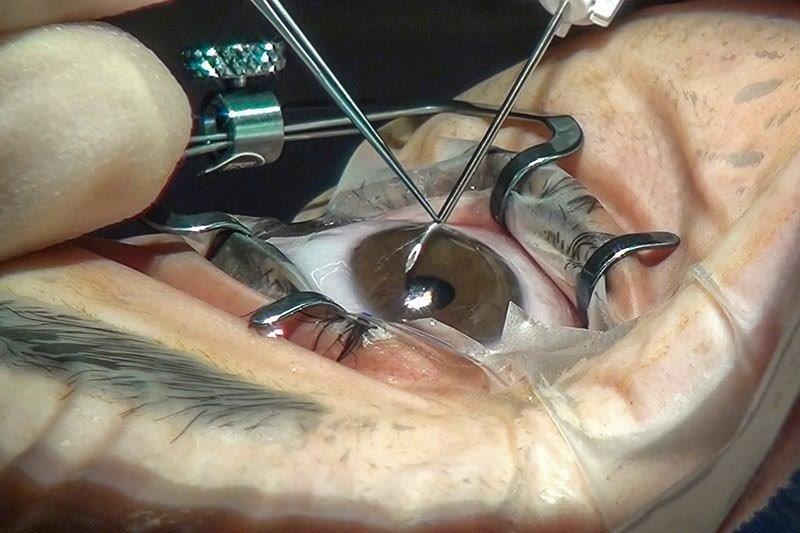
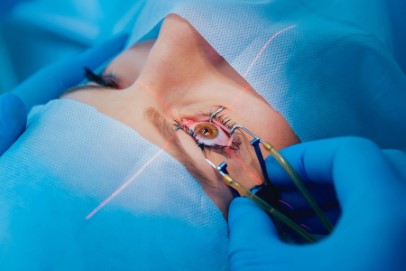
Common themes emerged, with 23.7% seeking general information about glaucoma, its complications and associated risks. Another 26.8% expressed interest in alternative treatment options, including eye drops, laser procedures, surgery and lifestyle advice. Almost a quarter of patients (23.7%) sought guidance on proper eye drop instillation techniques and aid devices, while 7.2% desired more information on medication side effects, with other concerns related to seeking reassurance about visual loss, understanding its implications for the future, the involvement of the other eye and various forms of support. Of the respondents, 41.1% were aged 71 and above; this age group may face challenges in seeking resources independently. This emphasises the significant role of acquiring information primarily through their direct healthcare provider.
The survey indicated a strong appreciation among patients for the services provided by GNZ, particularly its newsletters, webinars, websites and phone calls. Notably, 13.3% of patients reported facing barriers to accessing clinics or appointments and 10% experienced disruptions in their care due to Covid-19, including being lost to follow-up.
Conclusions and next steps
Our study faced limitations due to a small sample size – limited to GNZ patients with telephone access – and potential biases from subjective reports. Objective measurements are necessary for a more accurate assessment of adherence barriers in the New Zealand healthcare setting. Despite these constraints, our findings provide valuable insights into the diverse informational needs of our patients. This information guides GNZ in developing tailored education and communication strategies, addressing knowledge gaps and enhancing overall patient support.
Building on the insights gained from the literature review and survey, GNZ is committed to ongoing surveys aimed at pinpointing areas where resources should be directed for the development of personalised support materials. Our goals include identification of non-adherence and understanding individual barriers, providing continuous education, correcting misconceptions and addressing anxieties associated with glaucoma. Our aim is to empower patients in managing their glaucoma through interventions tailored to patient needs; these encompass strategies including telehealth, written information, online videos, community support groups and educational conferences.
It is important to recognise that glaucoma education should extend beyond patients with established disease. Early detection is key for better intervention and prognosis, requiring a broader understanding among the public, similar to conditions such as hypertension and diabetes. We actively encourage all healthcare providers to participate in raising awareness of glaucoma in their communities and to refer patients to GNZ for appropriate support.
Acknowledgements
The author would like to thank Professor Helen Danesh-Meyer and Pippa Martin, chair and general manager of GNZ, respectively, ophthalmology registrar and honorary research fellow Dr Ruhella Hossain and medical student Elena Edgar-Nemec.
References
- Tham Y, Li X, Wong T, et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–2090.
- Burton, Matthew J et al. The Lancet Global Health Commission on Global Eye Health: Vision beyond 2020. Lancet Glob Health 9.4 (2021): e489–e551. Web.
- World Health Organization. Adherence to long-term therapies: Evidence for action. http://apps.who.int/medicinedocs/pdf/s4883e/s4883e.pdf.
- Tsai J, McClure C, Ramos S, et al. Compliance barriers in glaucoma: a systematic classification. J Glaucoma. 2003;12:393–398.
- Taylor S, Galbraith S, Mills R. Causes of non-compliance with drug regimens in glaucoma patients: a qualitative study. JOculPharmacolTher. 2002;18:401–409.
- Patel S, Spaeth G. Compliance in patients prescribed eyedrops for glaucoma. Ophthalmic Surg. 1995;26:233–236.
- Danesh-Meyer H, et al. What do people with glaucoma know about their condition? a comparative cross-sectional incidence and prevalence survey. Clin Exp Ophthalmol 36.1 (2008): 13–18. Web.
- Gray T, Fenerty C, Harper R, Spencer A, Campbell M, Henson D, Waterman H. Individualised patient care as an adjunct to standard care for promoting adherence to ocular hypotensive therapy: an exploratory randomised controlled trial. Eye (Lond) 2012;26:407–17.
- Waterman H, Evans J, Gray T, Henson D, Harper R. Interventions for improving adherence to ocular hypotensive therapy. Cochrane Database Syst Rev. 2013;CD006132.
- Ha A, Jang M, Shim S, Kim C, Chang I, Kim Y (2022). Interventions for glaucoma medication adherence improvement: a network meta-analysis of randomized controlled trials. Ophthal. 2022 Nov;129(11):1294-1304.

Esther Kim is a final year medical student with the University of Auckland who has been volunteering at GNZ as a clinical educator since 2022. She undertook a summer studentship, under the supervision of Prof Helen Danesh-Meyer, on the role of communication and education in glaucoma medication adherence.