Humanising digital health connections
When I think about digital health, I think about technology, data, population health, AI and innovation. But arriving at Hamilton’s Claudelands Events Centre for HiNZ (Health Informatics New Zealand) Digital Health Week, little did I know the central theme would be a resounding chorus of "people, people, people". As the Māori proverb goes, ‘He aha te mea nui o te ao? He tangata, he tangata, he tangata!’ (What is the most important thing in the world? It is people, it is people, it is people!). In his insightful keynote, Brian Biggs, director of Auckland’s InterSystems, reminded us of this theme, stressing that digital transformation is so much more than just adapting our healthcare software.
The HiNZ Digital Health Week conference began with a karakia, sending chills down the spines of more than 1,200 attendees. It also served as a poignant reminder that the land we tread upon is not our own, emphasising the need to uphold Te Tiriti o Waitangi as we collectively move forward. Overarching themes encapsulated equity in healthcare, interoperability, codesign and embracing change, all from a resolutely people-centered perspective. HiNZ CEO Tim Corbett offered a compelling narrative, depicting New Zealand as a unique space for digital health, deeply rooted in the values of the Treaty. We were mesmerised by a sand artist who narrated this story by ‘weaving’ individual strands into a whare and a mat to meet upon to bring about a truly connected but broad ecosystem.

Keynote speaker Brian Biggs
Ngahihi o te ra Bidois, author and professional leadership speaker, discussed our responsibility to become exemplary ancestors for future generations. Proudly acknowledging that everything he’s achieved in life was because of the people around him, he concluded with a powerful haka, leading to many appreciative murmurs and reiterating the importance of the human element while we endeavour to change our digital health system.
Breaking down silos
Change in digital health is inevitable, said Biggs. The senior leadership team at Te Whatu Ora appeared to enthusiastically agree, while discussing the mountain of work ahead of them to achieve this change in both technology and mindset on how data can and should be used. It was interesting to be reminded, however, that although the pandemic forced us into using telehealth more widely, it’s been around for decades.
Dr Angela Lim, CEO of mental health startup Clearhead, spoke about breaking down the silos in our complex health systems and the company’s new AI-driven mental health app, designed to help do just that. Michael Draheim, chief clinical information officer at cloud-based data solutions company Oracle, addressed how often health records are written on paper and the urgent need to move everyone to digital to connect records with people wherever they are. Other companies, such as Noted, Manage My Health and Valentia Technologies, have been exploring this, with interoperability a key theme of the conference and in the exhibition hall.

Dr Angela Lim, CEO of Clearhead, discussing the impact being made in mental health
In the web of healthcare, we have all experienced the frustration of broken processes, so it was no surprise to hear comments about this throughout the conference. Whether it’s the constant retelling of our health concerns to different staff at our GP or hearing information second-hand through a family member going through the hospital system for a simple surgery, the banks of health information in Aotearoa’s healthcare system do not seem to talk to each other.
The fact that healthcare services and information have traditionally operated in silos was widely acknowledged, as were the barriers of funding constraints and privacy concerns, which have hindered the establishment of a seamlessly integrated system of care. The difficulties in sharing data between the public and private sector were also reiterated. For example, HealthOne, a shared electronic database, allows GPs and other healthcare professionals to easily access patient information. However, if an optometry practice used it, the patient’s record would only show they had attended an optometry appointment, without any relevant clinical information.
How much better would it be if a clinician could obtain a wider view of a patient’s health than just what they can gather at an appointment? A singular source of information would not only streamline internal processes but also facilitate smoother communication with other healthcare providers. This would reduce many laborious tasks in the process, reduce mistakes and optimise health data use, transforming the healthcare landscape and laying the foundations for more accurate diagnoses and treatment. This was exemplified by the presentation on the successful implementation of a clinical documentation improvement programme at Auckland City Hospital, led by nurses who wanted to shift the focus of care to quality improvement in patient records.
Staff from Te Whatu Ora spoke of the Hira programme (see story p16), which should be completed around the end of 2026 and will enable information to be pulled from different systems to create a personal health record for each and every patient. A representative at the Te Whatu Ora booth assured me that optometry would be part of the second tranche of Hira. It will be interesting to see how this unfolds, however, following our recent change in government.
Another obstacle is the digitisation of clinical records, including a patient’s historical data to provide a comprehensive view of their health, all of which will require careful consideration, strategic implementation and a great deal of work.
Codesign, practicality and trust
Codesign also emerged as a pivotal concept. “If tools are useful, people will use them,” said Adjunct Professor Robyn Whittaker, Te Whatu Ora’s director of evidence research and clinical trials. She explained that the global shift toward consumer-centered design challenges the healthcare system to think about the end users and their journey, as well as collaborating with subject-matter experts and the people in power (those who hold the purse strings) as part of the process. It’s not enough to make technology accessible – it needs to be trusted, she said, stressing that transformation is a collective effort, rooted in the collaborative strength of teams rather than individual endeavour.
Discussions on Māori data sovereignty highlighted the delicate balance between innovation, speed and regulatory compliance. Niru Rajakumar, VP Asia-Pacific at Orion Health, pointed out that 30% of the world’s data by volume is healthcare data, which is predicted to grow faster than any other data type. However, as much as 97% of that data is not currently being used. Think about all the valuable insights we can find out about the health of people and our communities if we put that to better use!


Orion Health’s Niru Rajakumar and (right) fellow speaker Dr Annick Jansen
Another highlight was the heartwarming presentation by Dr Annick Jansen, a research associate from Victoria University, who touched on accessibility for minorities. She spoke about using a strength-based approach rather than the current deficit-orientated model for our disabled communities. “With good technology, they can go so much further in their journey,” she said.
Overall, I left the conference excited to know that our country’s health technology thought-leaders have people at the forefront of their endeavours. As Rukingi Haupapa from Awhi Mai Stroke Charitable Trust said, “Barriers can get in between people. It’s the human touch that can change everything.” Integrated health data makes sense, but it was clear from this year’s HiNZ conference that the practicalities of implementing such a system are still complex and daunting.

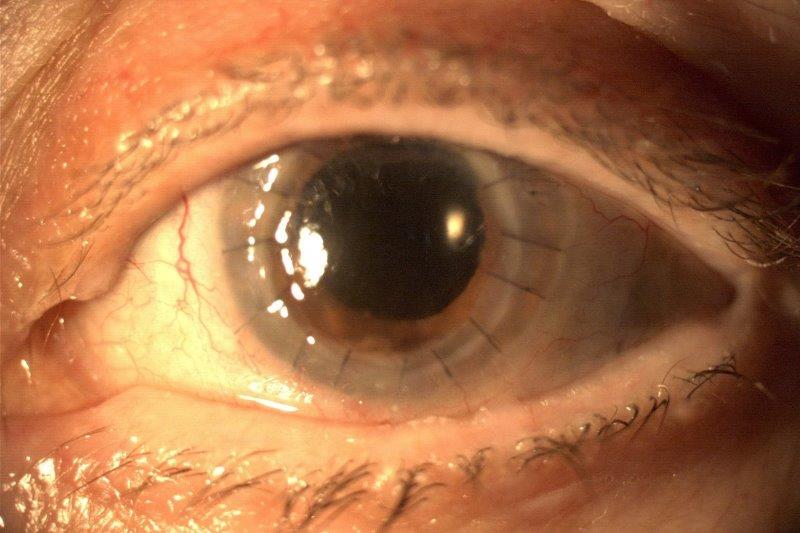
Neelam Mistry has worked in medical device AI within eyecare for nearly five years. Her master’s thesis investigated a technique to measure the viscosity of the vitreous humour with laser pulses using optical coherence elastography (a variant of OCT).