Retinal research and uveal melanoma
Overall survival benefit with tebentafusp in metastatic uveal melanoma
Nathan P, Hassel J, Rutkowski P, Baurain J, Butler M, IMCgp100-202 Investigators
N Engl J Med 2021, 23;385:1196-1206
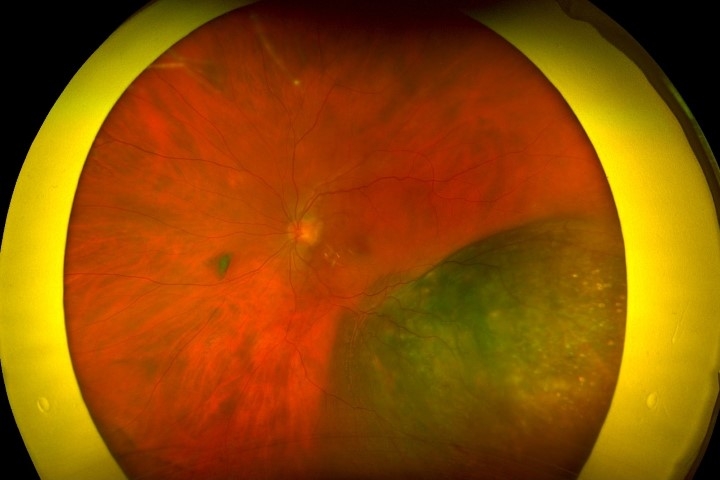
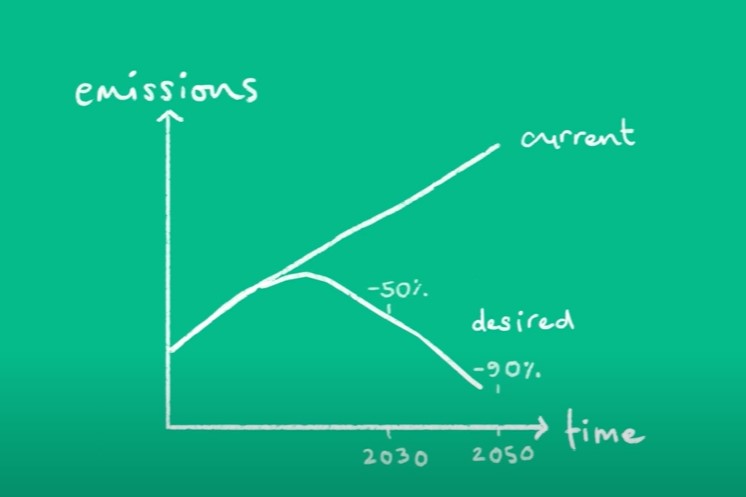
Review: Currently, there is no evidence of survival benefit with systemic therapy for metastatic uveal melanoma, with a one-year overall survival rate of 50%. The bispecific protein tebentafusp (Kimmtrak) consists of an affinity-enhanced T-cell receptor which fuses to an anti-CD3 effector that directs T-cells to target HLA-A*02:01 glycoprotein 100–positive cells (Fig 1, above).
This randomised, open-label, phase 3 trial included 379 patients with previously untreated metastatic uveal melanoma who were positive for the HLA-A*02:01 allele. In total, 252 received tebentafusp, while 126 received single-agent therapy with pembrolizumab (Keytruda), ipilimumab (Yervoy), or dacarbazine (DTIC-Dome) as the control. The overall survival at one year was 73% in patients with tebentafusp, compared with 59% in controls, while progression-free survival was also better (Fig 2). Among those receiving tebentafusp, 83%, 76% and 69% reported T-cell and cytokine-mediated adverse events, including rash, pyrexia, and pruritus, respectively, with 2% discontinuing the trial. No treatment-related deaths were observed. Despite antibodies against tebentaufsp being detected in some patients, the authors did not find they affected overall survival.
Comment: Approximately 45% of Caucasians in the US and Europe carry the HLA-A*02:01-allele, with a reported prevalence of 6-22% among specific populations in New Zealand. Considering the lack of effective systemic therapy for metastatic uveal melanoma, the results of this study are encouraging, with tebentafusp resulting in improved overall survival with an acceptable safety profile.
Factors associated with good visual acuity outcomes after retinectomy in eyes with proliferative vitreoretinopathy
Israilevich R, Starr M, Mahmoudzadeh R, Salabati M, Swaminathan V, Huang D et al.
Am J Ophthalmol 2022, 240:143-148
Review: Proliferative vitreoretinopathy (PVR) is the most common cause of failure of rhegmatogenous retinal detachment (RD) repair and affects 5-10% of cases. In situations where a scleral buckle and/or peeling of the preretinal or subretinal membranes are insufficient to reduce tractional forces on the retina, a retinectomy may be necessary. Eyes undergoing PVR repair have poor visual outcomes, with only 20% achieving >6/24 vision. The purpose of this retrospective, single-centre case-control study was to determine the factors associated with good visual acuity (VA) (>6/21) following repair of RD in eyes with PVR undergoing retinectomy.
Among the metrics compared were time to surgery for both primary and recurrent RD, lens status, size of the initial RD, macula involvement, PVR grade and retinectomy size. In the period between January 2015 and December 2019, 5,355 eyes were diagnosed, of which 345 had PVR and required a retinectomy. In the 'good vision’ cohort, 62 eyes had a mean final acuity of 6/12, whereas 119 eyes in the 'poor vision’ cohort had a mean final acuity of 6/208.
Several factors were found to predict good vision, including a smaller initial RD size (p=0.009), fewer surgeries (p=0.0002), a shorter interval between recurrent RD diagnosis and subsequent surgery (p=0.0006), better preoperative VA (p=0.0276), and pseudophakia at the final visit (p=0.005). The timing of subsequent RD repair after diagnosis of a redetachment appeared to be the single most important modifiable factor in favour of attaining good vision, driven by a shorter time to redo surgery when gas had been used at the prior surgery (1.2 vs 4.3 days; p=0.0047), more so than when silicone oil was present (5.9 vs. 7 days; p=0.70).
Comment: This study shows that good visual outcomes can be achieved in eyes with RD due to PVR requiring retinectomy. Some advocate delaying PVR surgery to allow the PVR process to become quiescent and the membranes to mature, making them easier to remove or peel. In spite of the retrospective nature of this study, the results raise the question of whether surgical intervention should be delayed in cases of PVR-related RD, particularly in the absence of silicone oil tamponade.
Four-year visual outcomes in the protocol W randomised trial of intravitreous aflibercept for prevention of vision-threatening complications of diabetic retinopathy
Maturi R, Glassman A, Josic K, Baker C, Gerstenblith A, Jampol L; DRCR Retina Network
JAMA 2023, 7;329:376-385
Review: In this study, investigators examined whether prophylactic treatment with aflibercept (Eylea) improved vision and anatomical outcomes in patients with non-proliferative diabetic retinopathy (NPDR) without centre-involving diabetic macular oedema (CI-DMO). It involved 399 eyes and 328 patients across 64 clinical sites in the US and Canada.
Patients received 2mg of aflibercept (every 16 weeks after three loading doses) over the first two years, followed by quarterly injections until year four, unless the eye improved to mild NPDR or better. Vision-threatening complications were also treated with aflibercept. At year four, there was a 33.9% cumulative probability of developing PDR or CI-DMO with vision loss in the aflibercept arm, compared to 56.9% in the sham arm (HR 0.40; p =0.01). The change in visual acuity from baseline to year four was not significantly different between the two groups (aflibercept -2.7 letters vs -2.4 sham; p=0.52).
Comments: Despite successful prevention of these complications at both years two and four, better visual outcomes were not observed at four years, compared to anti-vascular endothelial growth factor (anti-VEGF) treatment initiated after vision-threatening complications developed. The use of anti-VEGF may not be warranted in patients with NPDR without CI-DMO as a preventive measure.

Dr Riyaz Bhikoo is an ophthalmologist with fellowship training in ocular oncology, medical retina, cataract and vitreoretinal surgery. He works at Auckland Eye, Middlemore Hospital and Greenlane Clinical Centre.