The perils of corridor consultations
“Could you just take a look at Elizabeth*?” asked the clinic nurse, “She’s got a funny eye.”
Elizabeth is a theatre nurse who occasionally works with us on our hospital’s eye lists. Despite approaching a long weekend, the overbooked clinic running 30 minutes late and the expectation of further additions to Canterbury’s blepharitis epidemic, I agreed to take a look at the end of clinic.
“What’s up with you, then? I can’t even see which eye has the problem,” I quipped, utilising the well-known technique of inspecting from two metres away. “Oh, well, come into the clinic room and I’ll take a quick look.”
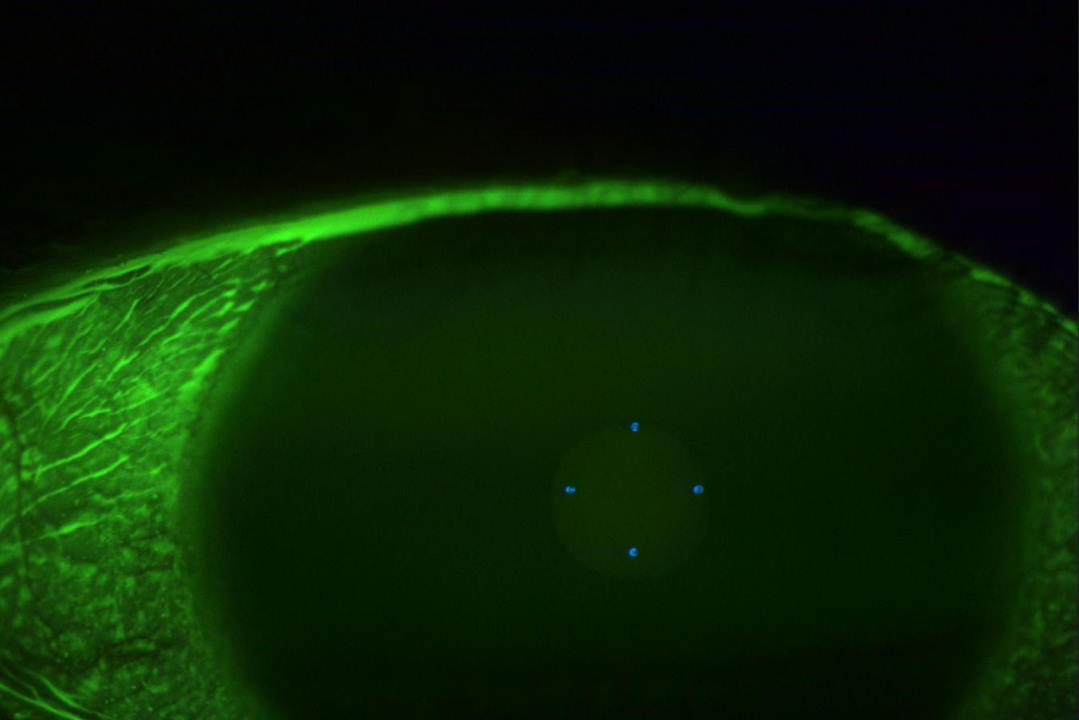
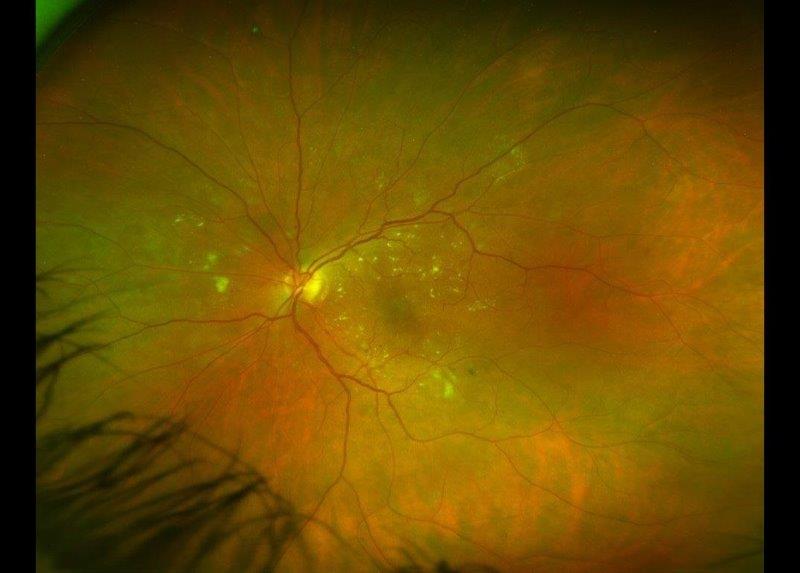
Working in a hospital with 500 employees, it’s not unusual for someone among the staff to have an eye problem. After a cursory history consisting of ‘eye’ and ‘not right’, I move to a slit-lamp examination, conveniently forgetting that all eye examinations begin with a visual acuity check. Fortunately, the trusty Haag-Streit BM900 comes to my rescue – proving that in this era of digital imaging technology and artificial intelligence, nothing beats old-fashioned optics and a bright light – for there in front of me, in Elizabeth’s left eye, is a cluster of keratic precipitates.

Elizabeth’s left eye (patient permission obtained)
I immediately backpedal and decide the conventional consultation approach is going to be better for all parties. Elizabeth registers formally as a patient on our system and we recommence the consultation with a history, visual acuity and intraocular pressure (IOP) check. As suspected, she appears to have a first episode of acute anterior uveitis with no obvious systemic associations. A prescription is generated, some photographs taken and a letter will be written to her primary healthcare provider detailing her diagnosis, as per best-practice recommendations.
Thus, these learning points came to mind:
- Staff in your workplace may have an eye problem and you could be ideally placed to diagnose and manage their condition
- Treat them as you would any other patient, by following the normal consultation process
- Document them as you would any other patient
- Communicate with other healthcare professionals involved in that person’s care
- Work within your accepted scope of practice and offer to refer elsewhere if necessary
Stay safe!
*not her real name

Dr Oliver Comyn is a cataract and vitreoretinal surgeon practising at St George’s Eye Care in Christchurch. Having trained in the UK, completing his doctor of medicine degree in diabetic eye disease research, he undertook a second vitreoretinal surgical fellowship at Moorfields and continues to be particularly interested in vitreomacular interface disorders.