Beware the cap wearer!
A 46-year-old male came for his first ever eye examination after noticing a patch of his left superior vision was missing and his vision was more blurry than normal. He reported no headaches, floaters or flashes and his eyes were otherwise comfortable. History included his maternal grandmother going blind due to an unknown cause and his mother possibly had a retinal detachment, but he wasn’t sure. He reported good health and was not on any medication. He came to his eye appointment wearing a cap, saying it was part of his “stylish attire”.
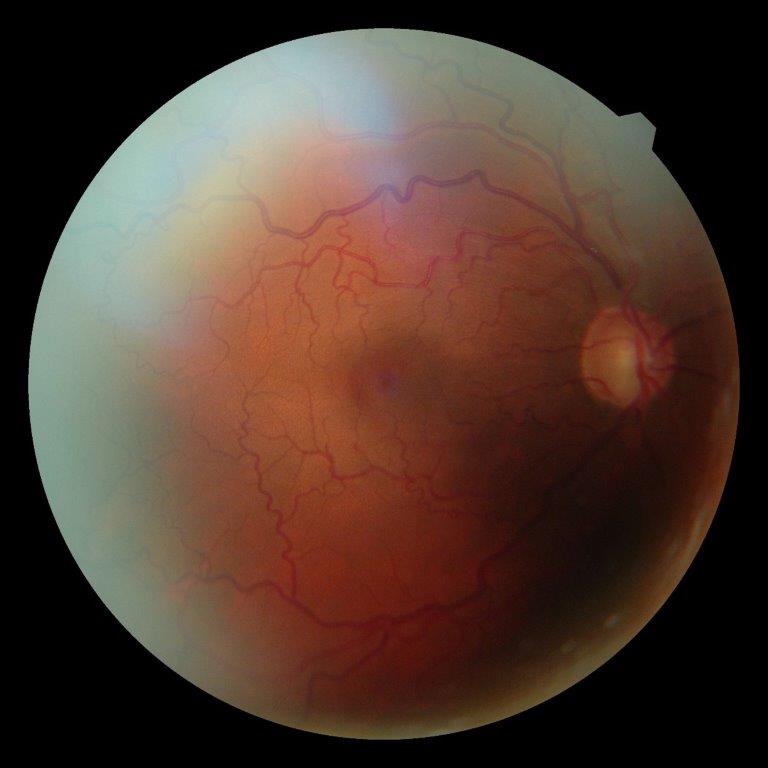
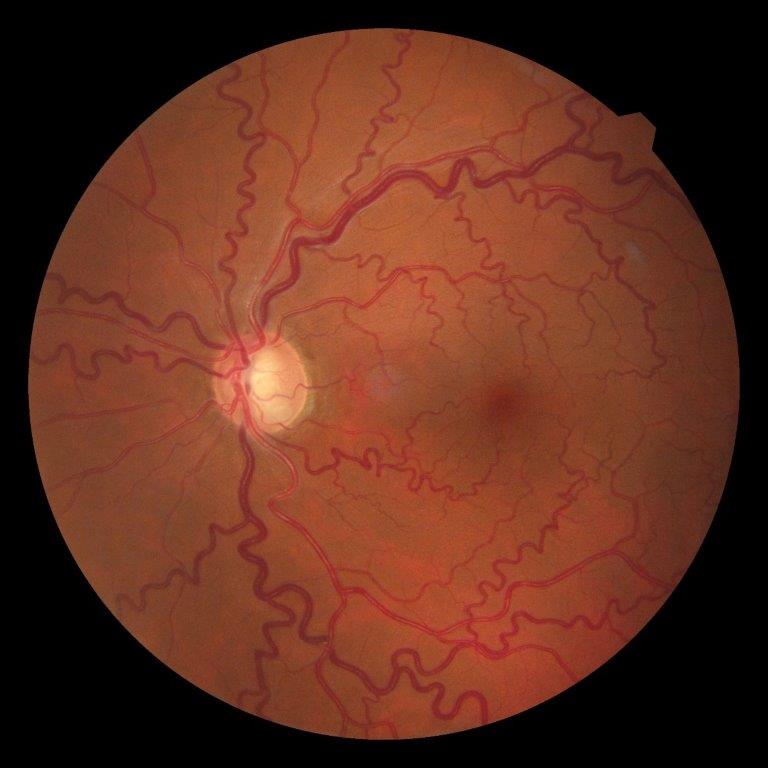
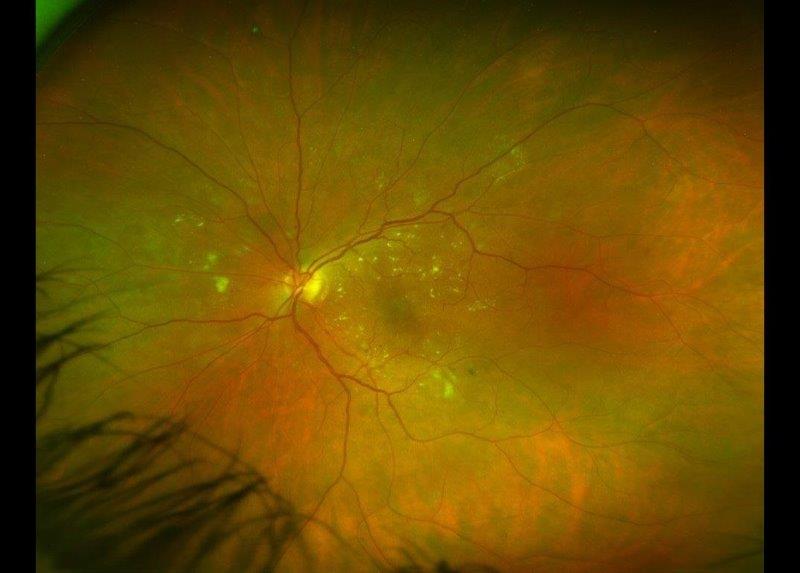
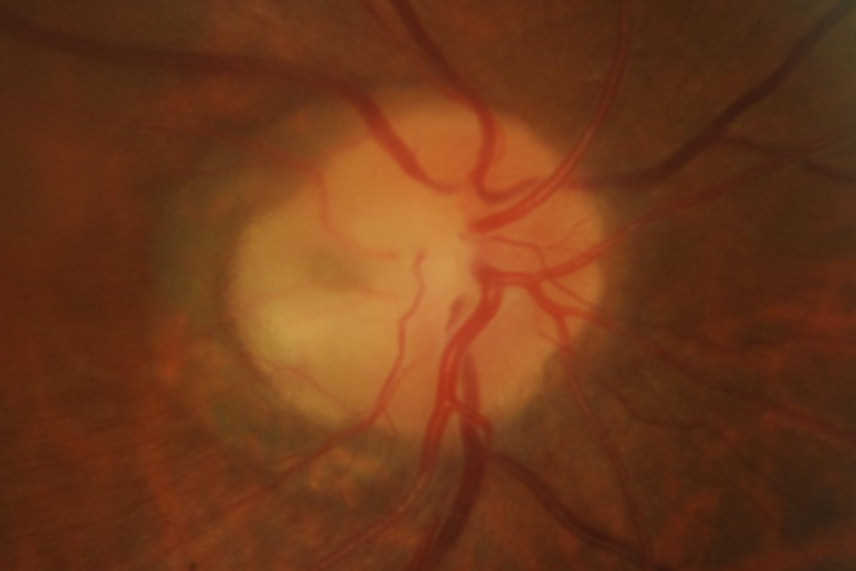
Fig 1 and 2: Right and left fundus, respectively
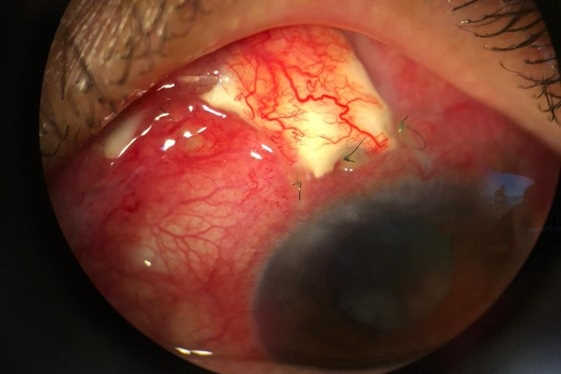
His uncorrected vision was right eye 6/6, left eye 6/7.5; refraction, right eye plano/-0.25 x 47, 6/6, with left eye -0.25/-0.25 x 170, 6/6. Slit-lamp examination showed narrow angles with gonioscopy in all four quadrants, both eyes. Cornea was clear, with no pigment dispersion syndrome or pseudo exfoliation material noted.
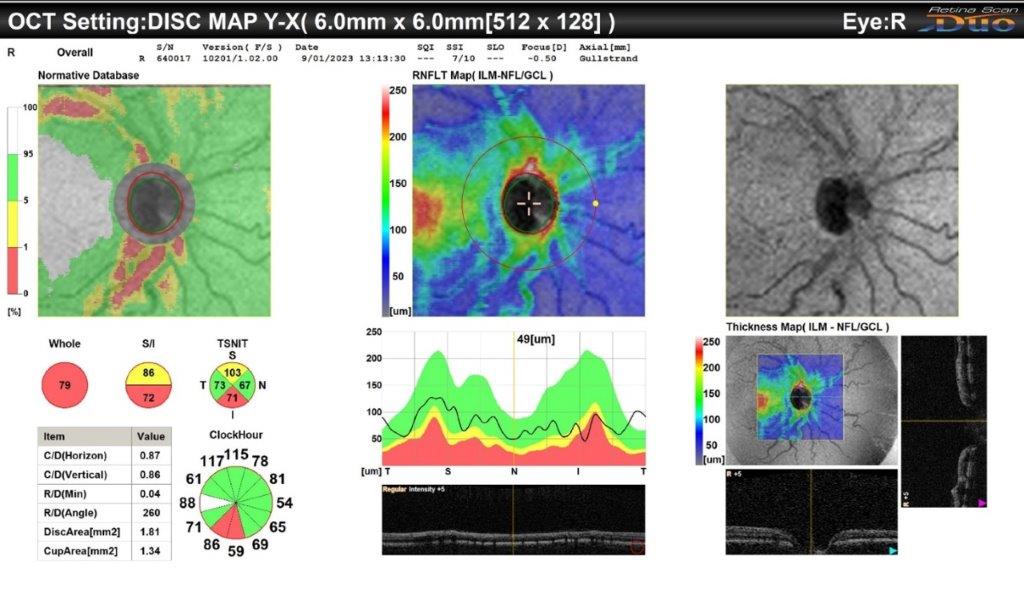
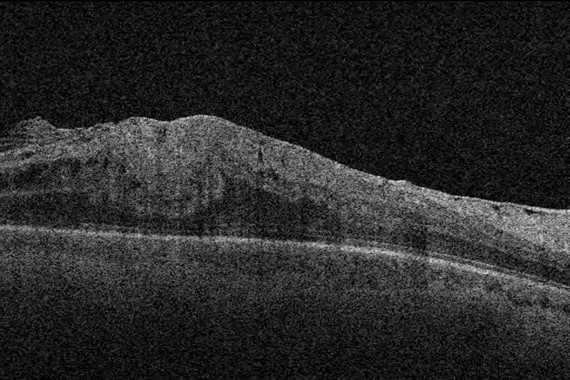
Fig 3. Right OCT showing significant loss on inferior neuroretinal rim
Fig 4. Left OCT Showing significant loss of superotemporal and inferior neuroretinal rim
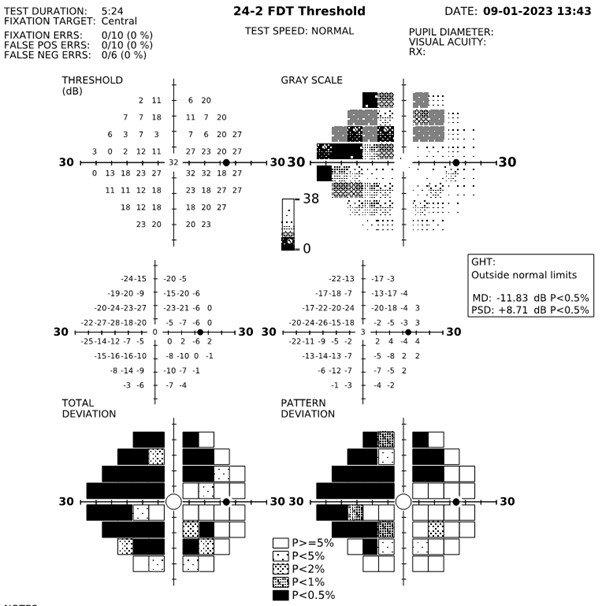
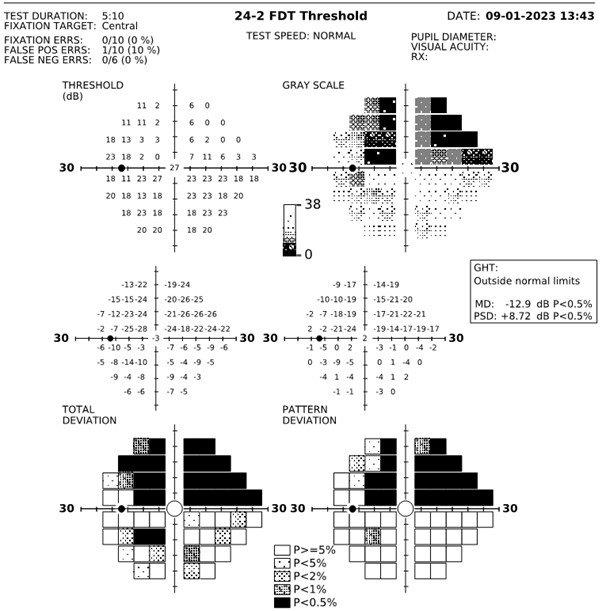
Fig 5 and 6. Right and left eye visual fields, respectively
Discussion
This interesting case highlights how habitually wearing a cap may impact how early a patient may detect a superior field defect. One wonders if he would have noticed his scotoma earlier had he not been wearing one. This finding may have implications for other headgear and demonstrates the importance of regular eye examinations, particularly if there is a family history of blindness or vision issues.
Another consideration is how little the public understands about their family history when it comes to eye disease. The fact that his grandmother went blind is significant but would have been much more meaningful for future generations had the diagnosis been known. Perhaps his grandmother also suffered from untreated chronic glaucoma – according to a study published in the International Journal of Environmental Research, 38% of respondents had not heard of the disease1.
It’s also worth noting a positive family history of an eye condition is significant, but a negative one does not necessarily mean it was not present, only that the patient believed it was not present. This is important to consider with conditions such as glaucoma and macular degeneration, where awareness of the disease is lacking. I advise my patients to make use of family gatherings to quiz family members on any significant health issues. While this goes against our cultural norms, it does help future generations’ awareness of possible health risks to aid early diagnosis.
Another key point from this case is the lack of symptoms from his occluded angles. So often we associate angle-closure glaucoma with eye pain, redness and decreased acuity. When narrow angle glaucoma is chronic, the classic symptoms of angle closure may not be present but, of course, the long-term ocular damage is permanent.
Looking at the photographs, there was significant tortuosity of his vessels. Despite his reporting good health and normal blood pressure, his GP was advised of my findings and a blood workup recommended.
Outcome
My patient was immediately referred to the Greenlane Superclinic, where he had four peripheral iridotomies performed that afternoon. He was also prescribed Travatan (travoprost), which, unfortunately, he reacted badly to. Consequently, he is investigating homeopathic treatment before going onto a different glaucoma drop.
Perhaps his homeopathic journey will be the topic of a future article!
Reference
- Int J Environ Res Public Health. 2023 Feb 17;20(4):3594.

Angela Garner is an optometrist and owner of Gates Eyewear in Newmarket, Auckland. She has a special interest in myopia control and pathology.